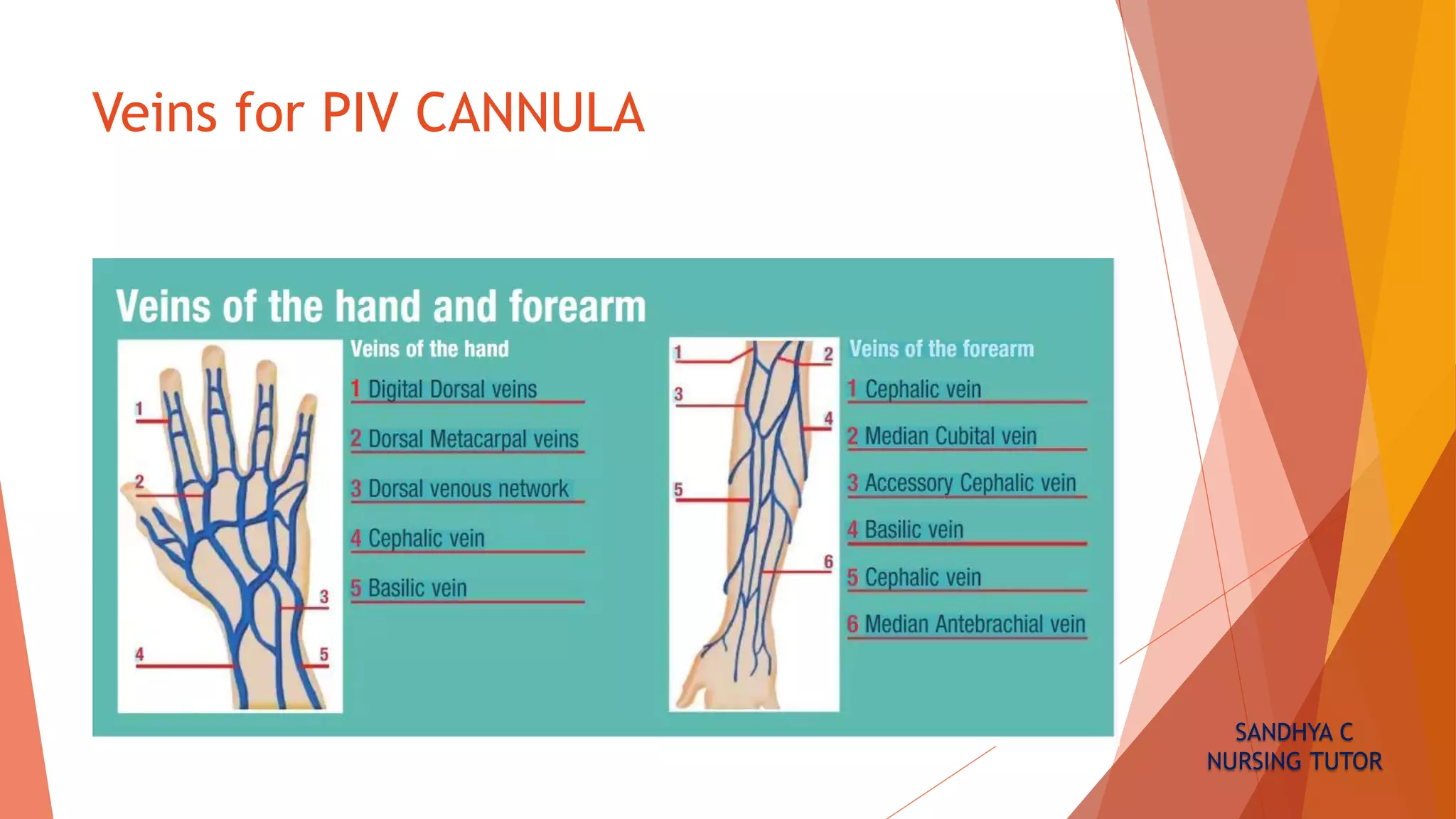
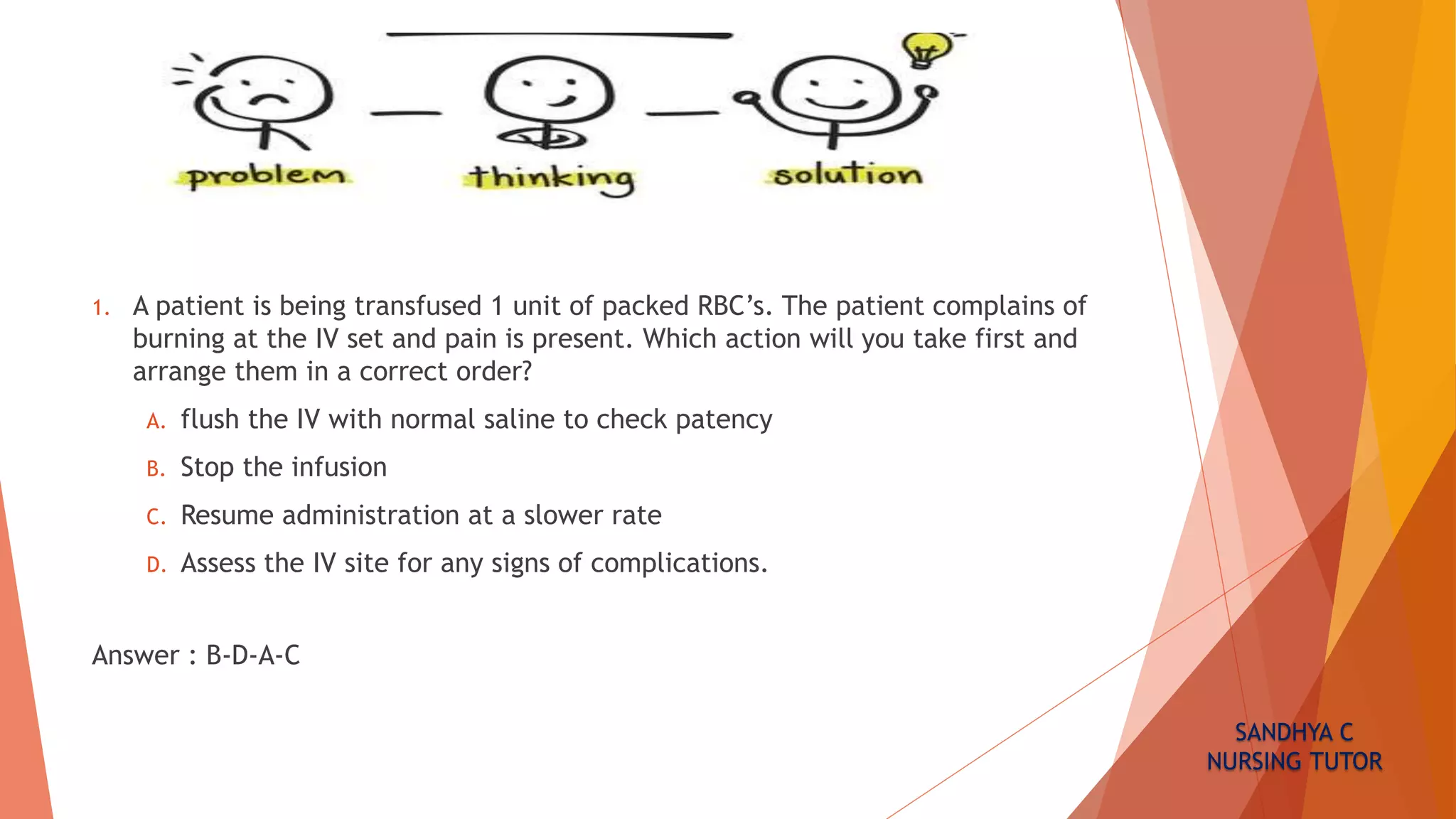
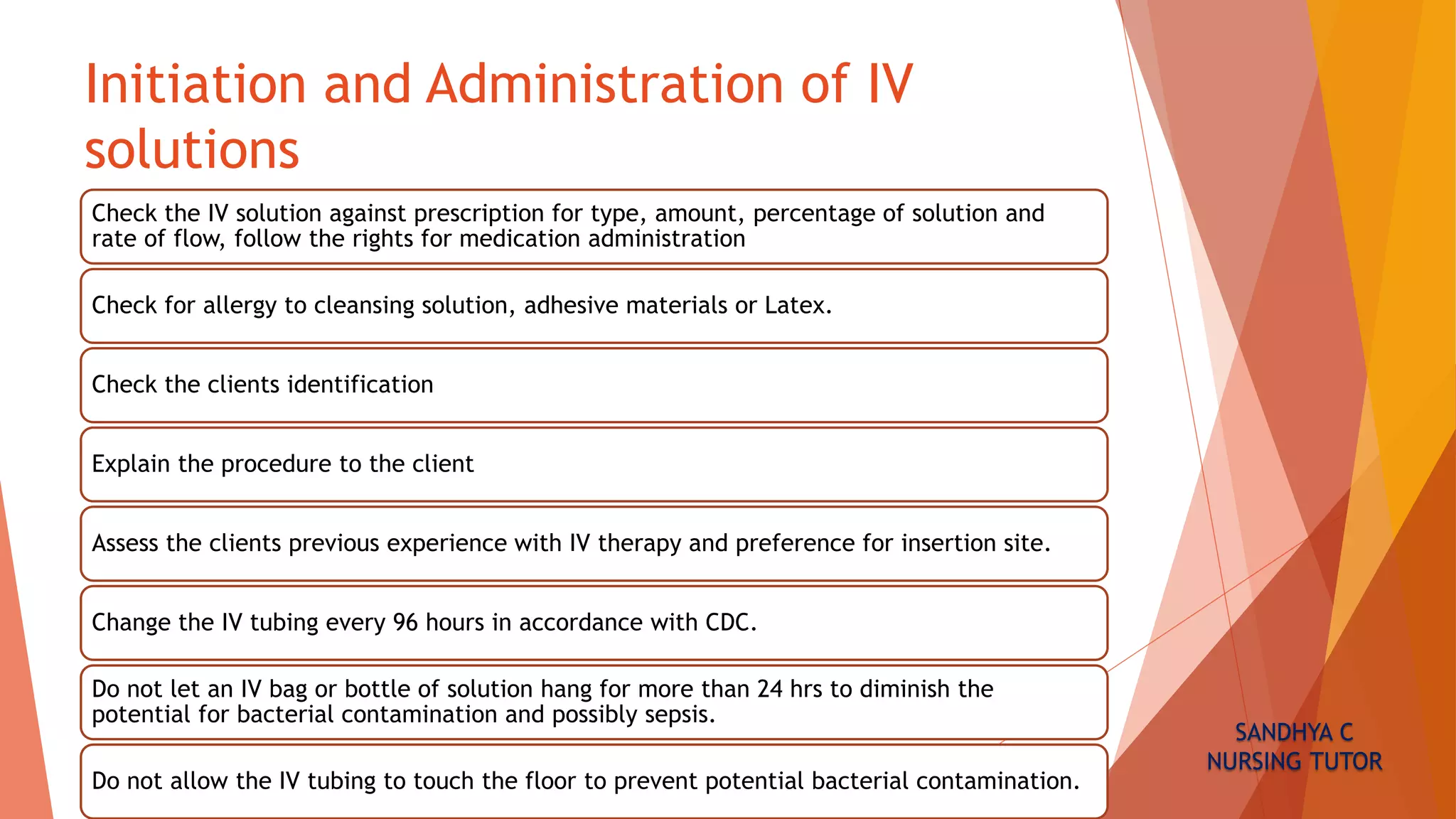
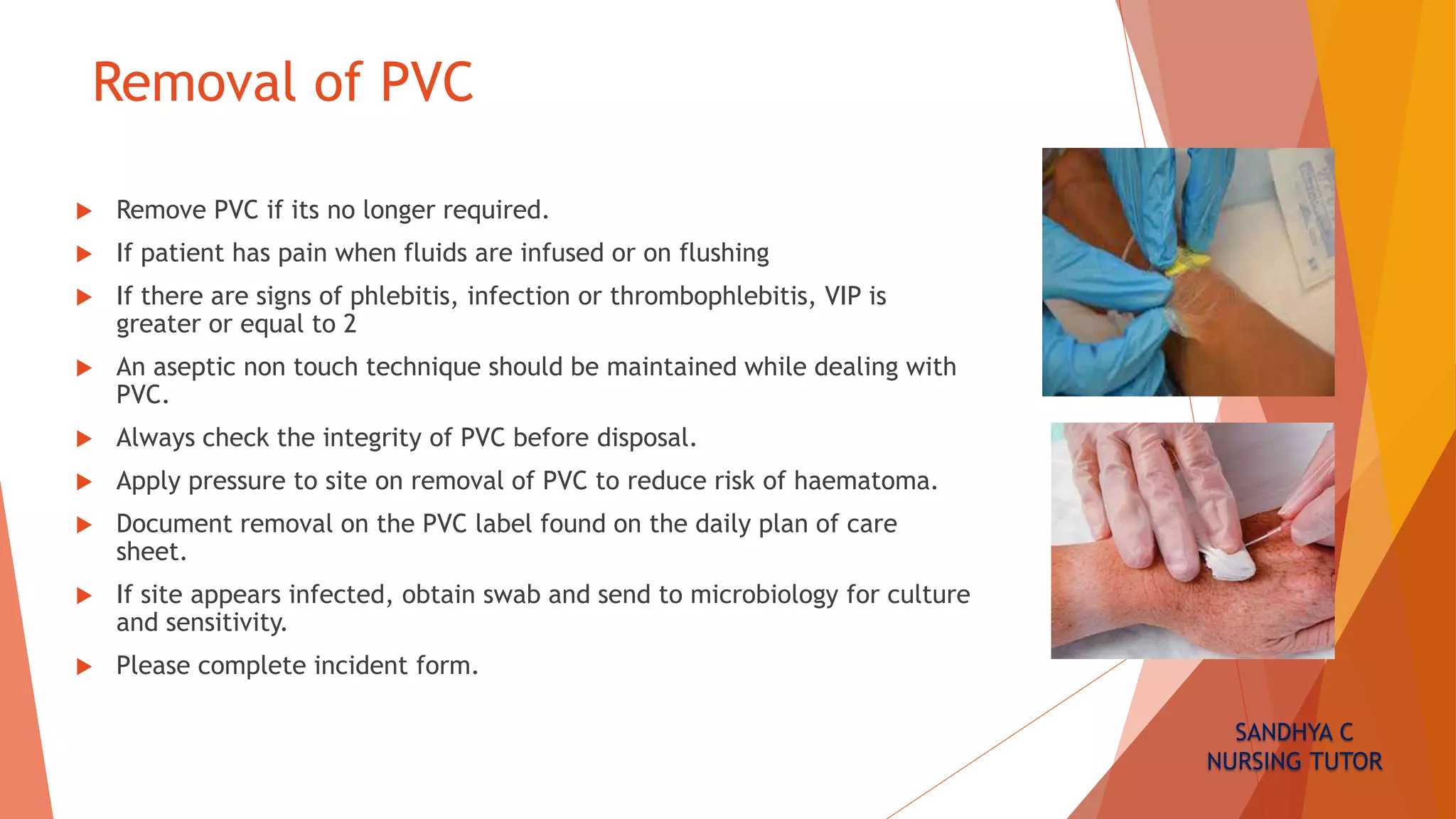
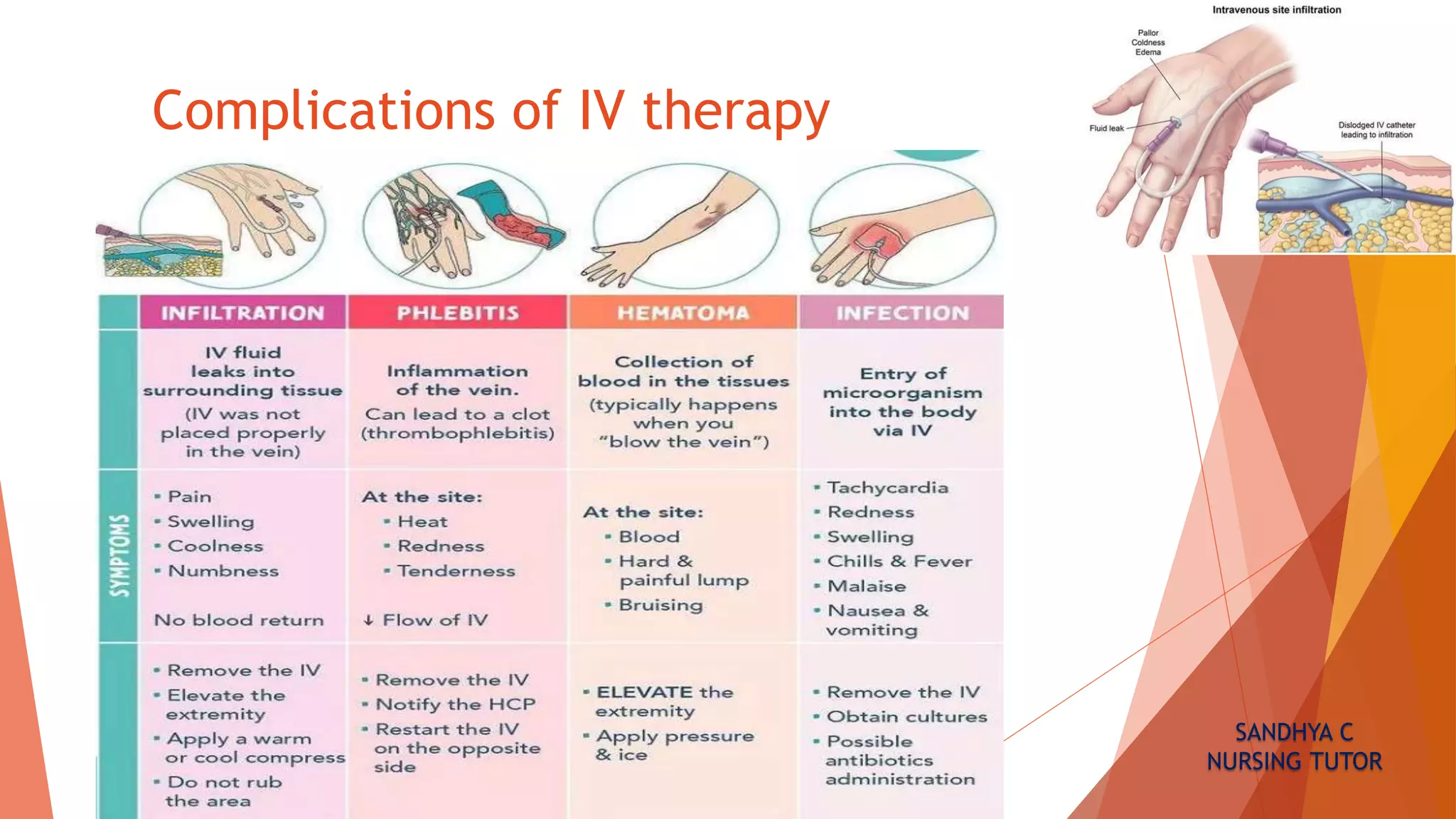
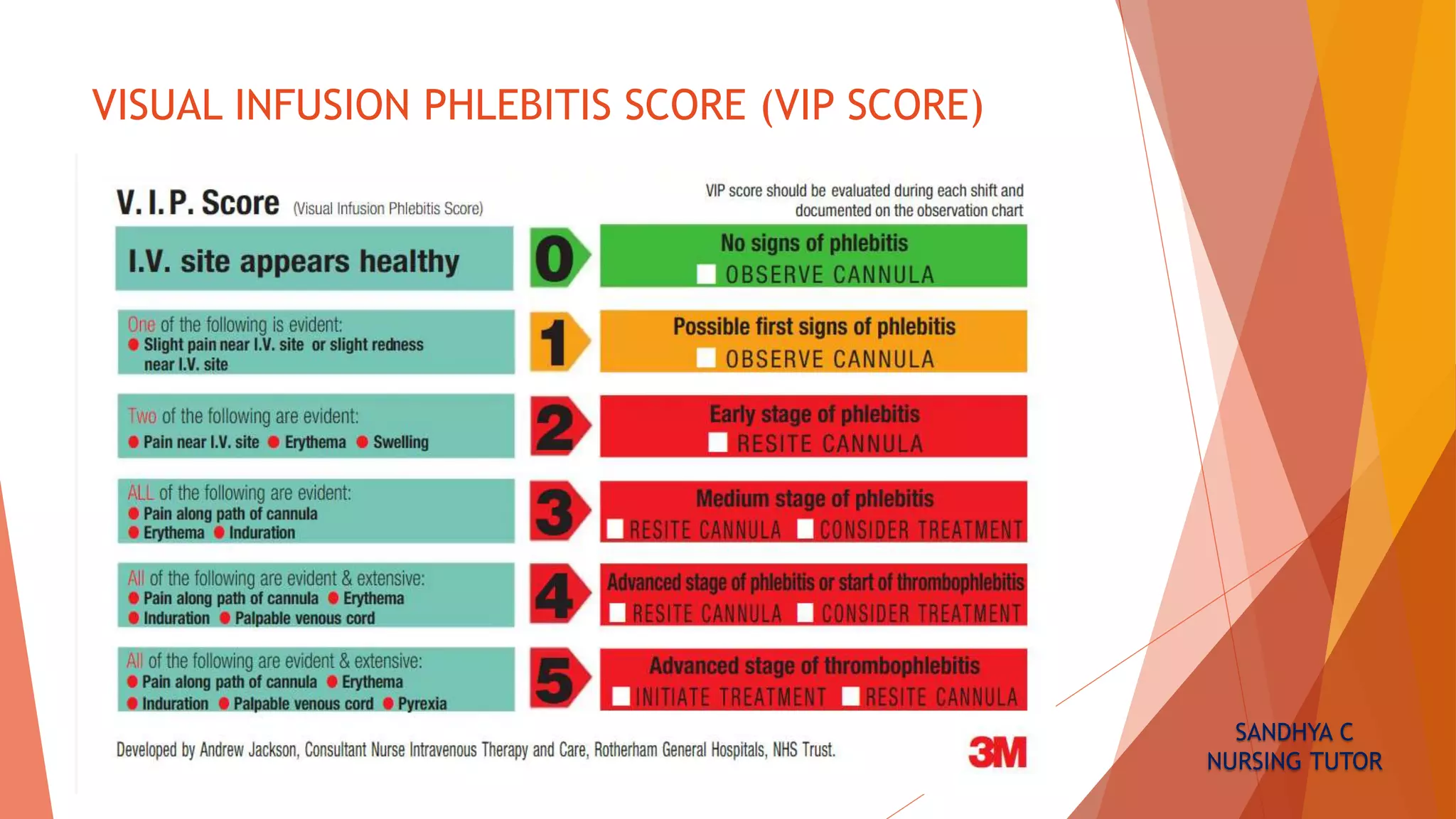
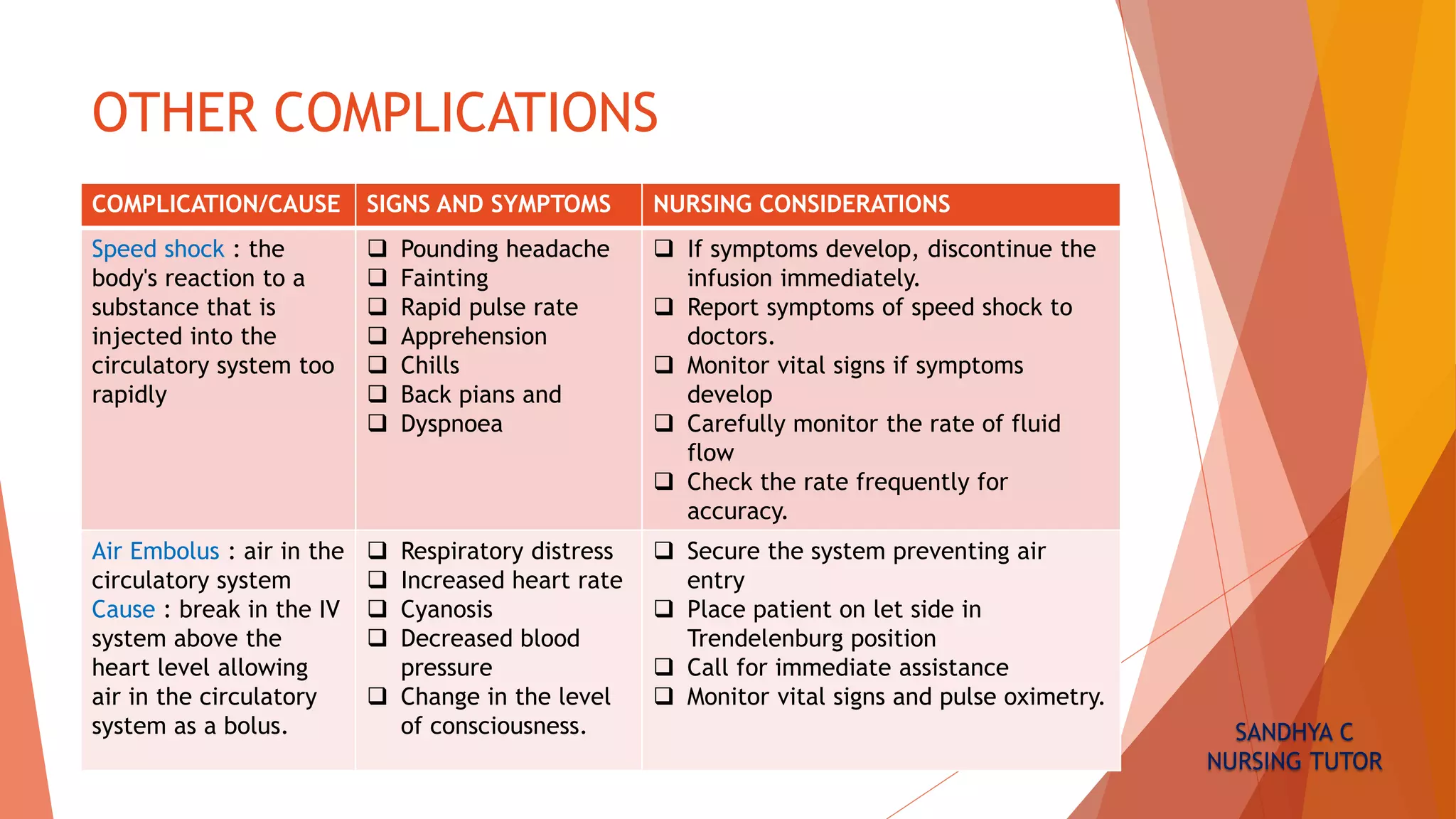
This document provides guidance on peripheral intravenous cannula care and assessment. It discusses appropriate sites for cannula insertion in adults and pediatrics. Ongoing care includes using aseptic technique for dressing changes and flushes. Signs of complications like infiltration or phlebitis should be monitored using the Visual Infusion Phlebitis Score. Removal criteria and potential complications are also outlined. Proper cannula care and assessment is important for newly graduated nurses who may lack hands-on experience starting peripheral lines.