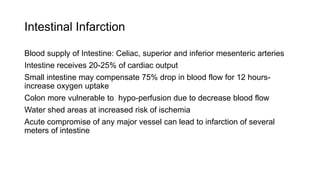
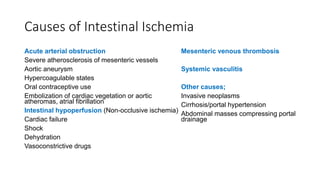
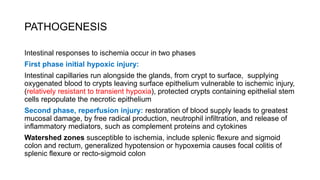
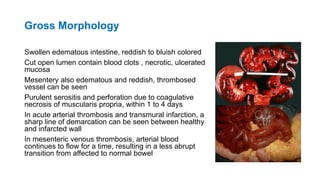
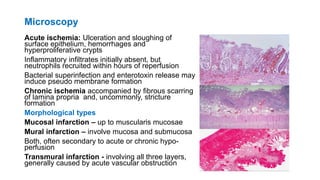
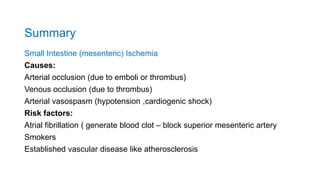
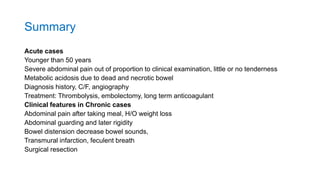
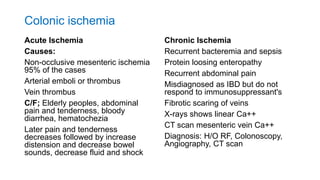
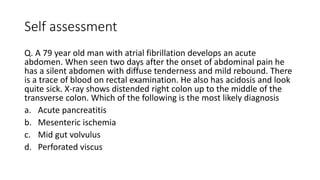
Intestinal ischemia can affect both the small intestine and colon. Acute small intestine ischemia is commonly caused by arterial occlusion from emboli or thrombus, while chronic cases are usually due to vasospasm. Risk factors include atrial fibrillation. Acute colonic ischemia typically affects elderly individuals and is often non-occlusive in nature. Clinical features include abdominal pain and tenderness as well as bloody diarrhea. Later findings include abdominal distension and decreased bowel sounds. Diagnosis involves history, exam, imaging studies, and angiography. Treatment involves thrombolysis, embolectomy, or resection depending on the severity and chronicity of the ischemia.