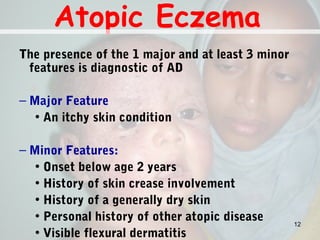
This document discusses various types of dermatitis and eczema. It begins with an introduction noting that dermatitis and eczema refer to inflammation of the skin. Eczema progresses through acute, subacute, and chronic stages. Prevalence in the US is 10-12% in children and 0.9% in adults, rising internationally. Atopic eczema is a chronic pruritic inflammation affecting the epidermis and dermis, commonly presenting in infants and children. Contact dermatitis results from allergic or irritant reactions to substances touching the skin. Other conditions discussed include lichen simplex chronicus, discoid eczema, seborrhoeic dermatitis, and

































![Contact Dermatitis [ CD ]
–Acute or chronic inflammatory reactions to
substances that come in contact with the
skin.
–Two forms of CD exist
• Irritant Contact Dermatitis (ICD)
• Allergic Contact Dermatitis (ACD)
39](https://image.slidesharecdn.com/dermatitisandeczema-130923012739-phpapp02/85/Dermatitis-and-eczema-39-320.jpg)
![Contact Dermatitis [ CD ]
• Common allergen-containing products include
• cosmetics
• Soaps
• dyes and
• jewelry.
• The most frequent sensitizers are
• fragrance
• nickel, neomycin
• formaldehyde, lanolin, and
• a host of other common environmental chemicals.
40](https://image.slidesharecdn.com/dermatitisandeczema-130923012739-phpapp02/85/Dermatitis-and-eczema-40-320.jpg)