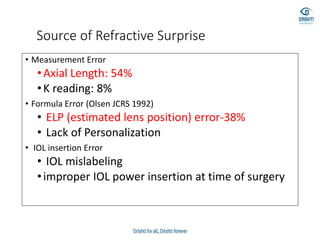
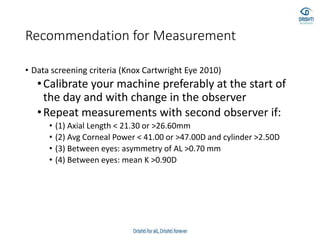
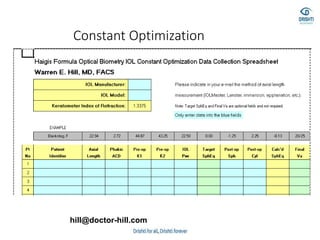
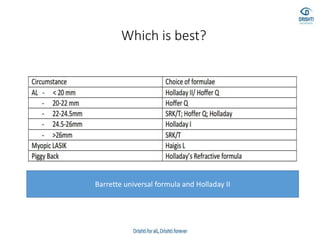
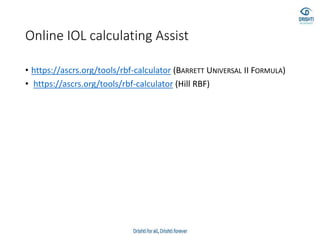
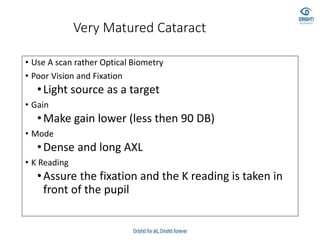
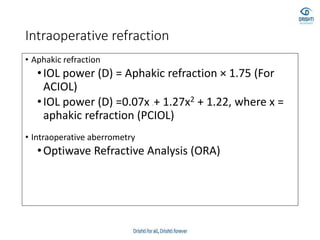
This document discusses various biometry techniques and considerations for accurate intraocular lens (IOL) power calculation in complex cases. It describes tools and methods for measuring ocular parameters in conditions like mature cataracts, posterior staphylomas, and post-refractive surgery eyes. Formulas for calculating IOL power for different IOL types and surgical procedures are presented. Intraoperative techniques like retinoscopy and aberrometry are also covered to optimize refractive outcomes.

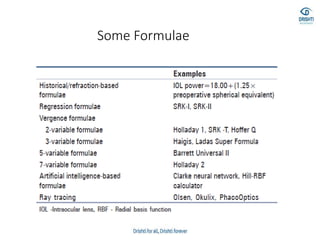
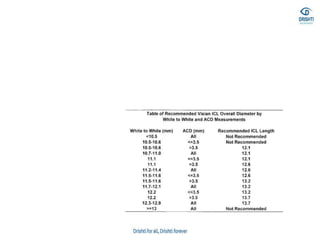
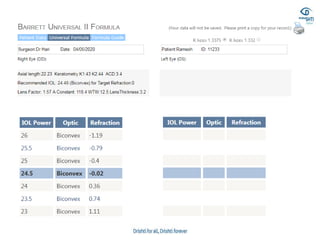
![IOL Formula
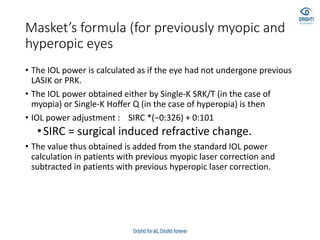
• SRK formula
• Calculated IOL: A-2.5L-0.9 K
• A: A constant (ELP)
• L: Measured Axial Length
• K: Average K reading
• Mathematical Formulae (Fyodorov and its
modifications)
• P = (1336/[AL- ELP]) (1336/[1336/{1000/([1000/DPostRx] - V) + K} - ELP])
• K: Net corneal power
• AL: Axial length
• P: IOL power
• ELP: Effective lens position
• DPostRx : Desired refraction
• V: Vertex distance](https://image.slidesharecdn.com/biometry-200908055813/85/Biometry-Not-only-a-mere-Measurement-26-320.jpg)
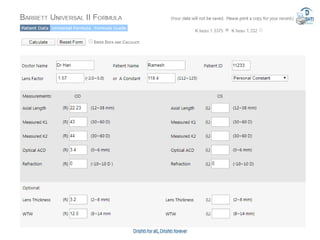
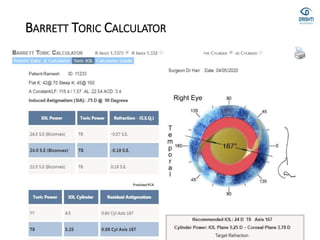
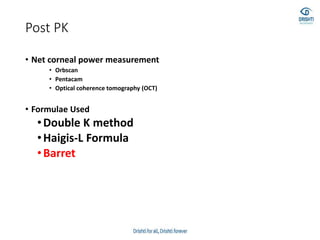
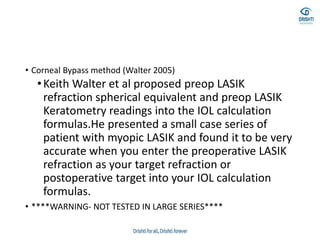

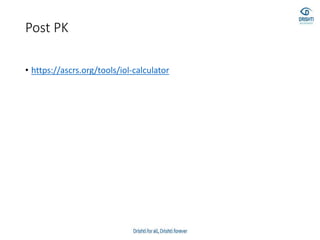
![• Barrett true-K no history formula
• This version of Barrett’s formula has been developed to
• work without historical data and can be accessed via the
• same websites reported for the “historical” version (see
• 2.1.4). The formula has not been published, but the results
• are good [33].](https://image.slidesharecdn.com/biometry-200908055813/85/Biometry-Not-only-a-mere-Measurement-64-320.jpg)