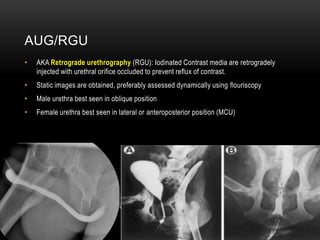
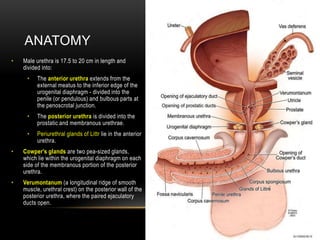
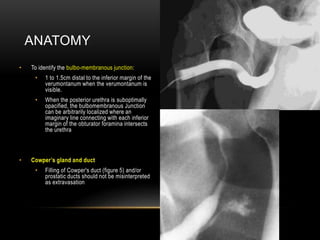
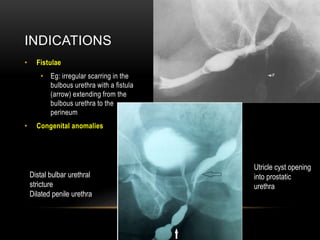
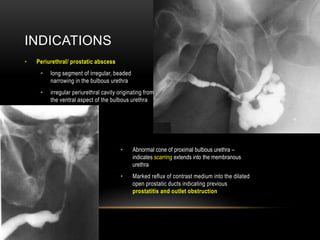
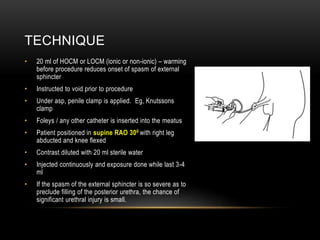
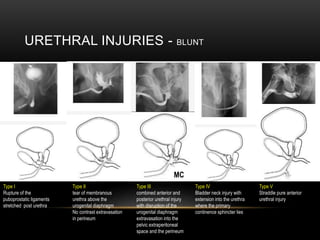
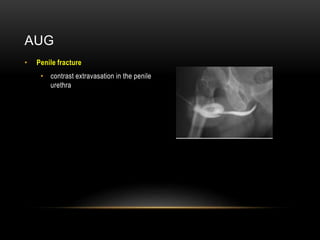
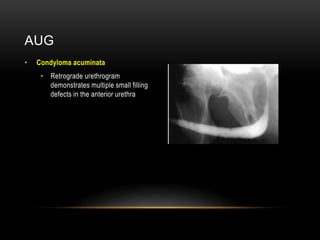
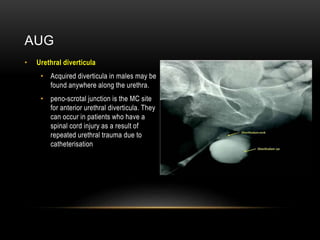
An ascending urethrogram (AUG) involves retrograde injection of iodinated contrast into the urethra to visualize its anatomy and identify any abnormalities. The male urethra is best seen in the oblique position while the female urethra is best seen laterally or anteroposteriorly. The AUG can detect urethral strictures, trauma, fistulas, congenital anomalies, periurethral abscesses, and tumors. Complications are rare but can include allergic reactions, urinary tract infection, and urethral injury. The AUG is useful for evaluating the type and extent of blunt urethral injuries as well as conditions like penile