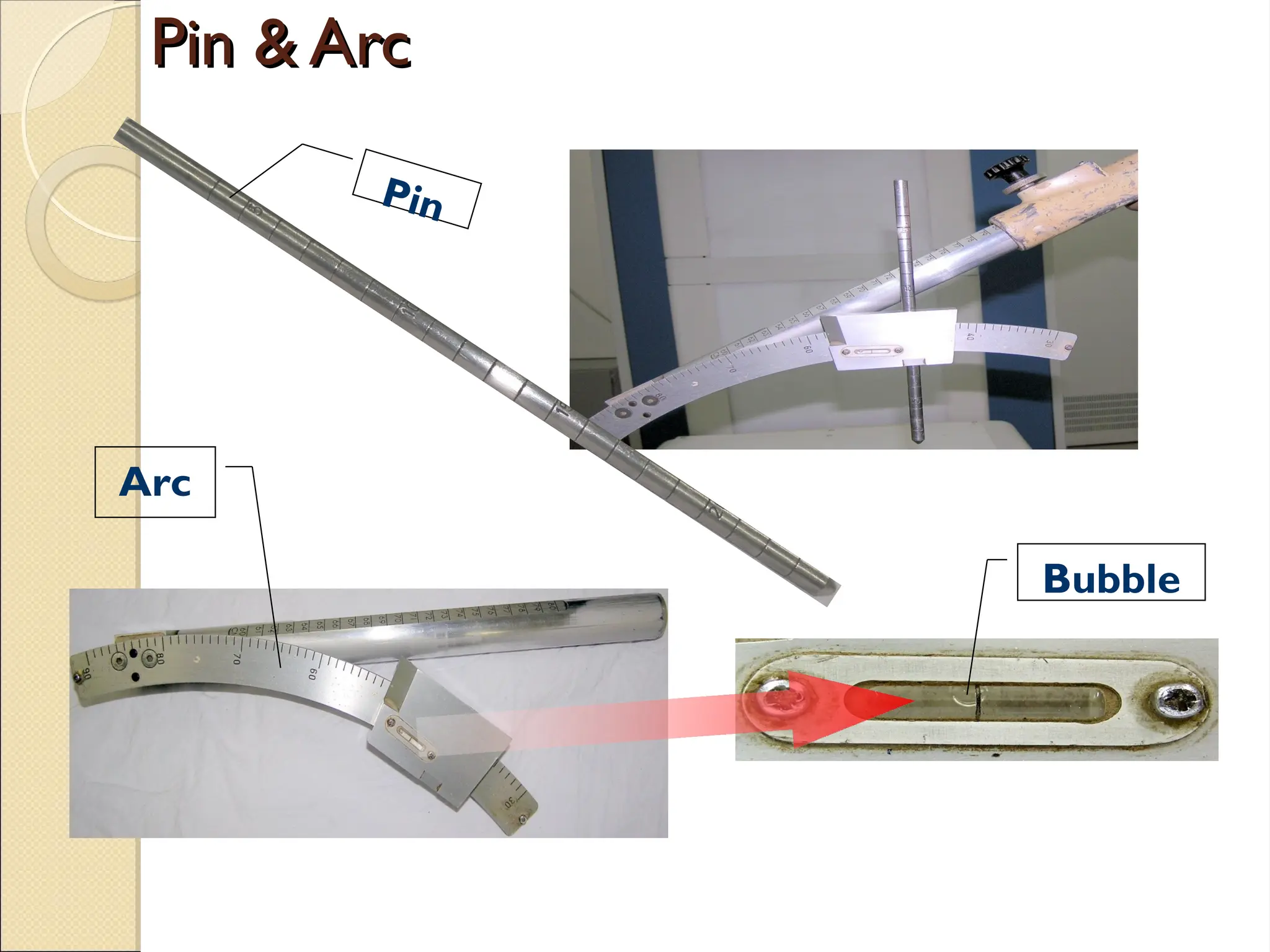
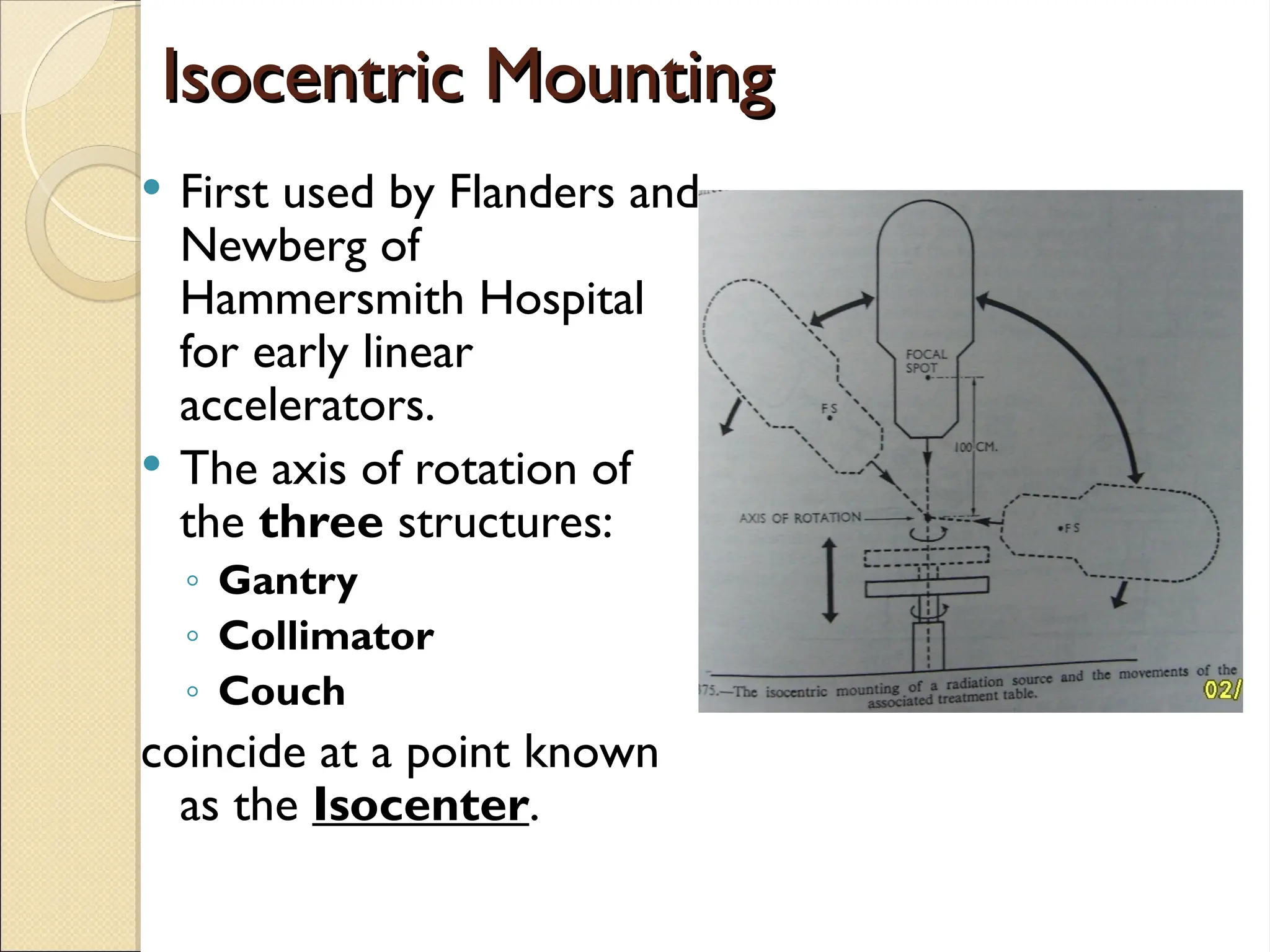
The document discusses the principles and practices of beam direction in radiotherapy, emphasizing the importance of precise localization and patient positioning for effective treatment. It outlines various localization methods, imaging techniques, and patient positioning aids to ensure accurate beam delivery while minimizing exposure to healthy tissue. Additionally, it addresses the types of radiation fields, treatment planning calculations, and verification processes to enhance the quality of radiation therapy.