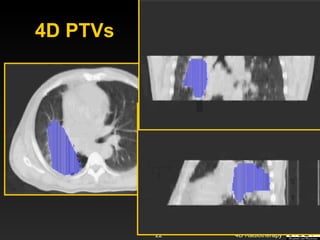
4D radiotherapy aims to account for tumor motion during radiation therapy by acquiring CT images over multiple phases of the breathing cycle (4D CT imaging) and using this information for treatment planning and delivery. It allows for more accurate targeting of tumors in organs affected by respiratory motion like the lungs. While 4D radiotherapy provides advantages over existing motion management techniques, there are still technological challenges and limitations like complexity, treatment time, and residual motion. Future work includes addressing these issues and further integrating 4D techniques with other advances in radiation oncology.