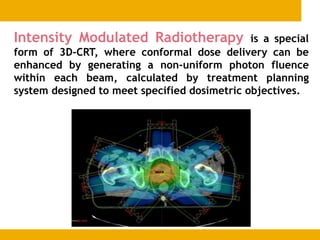
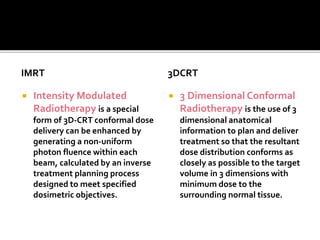
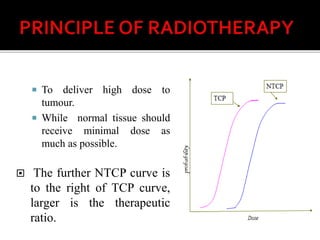
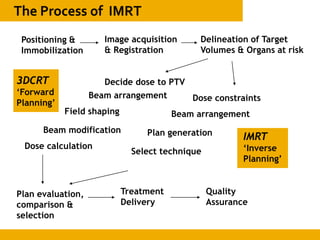
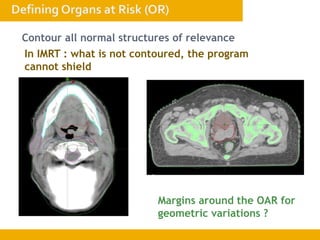
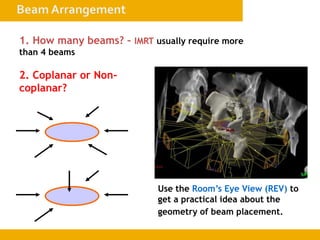
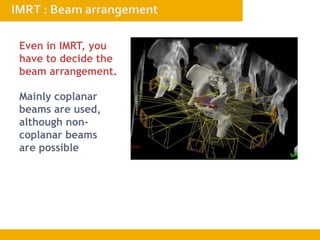
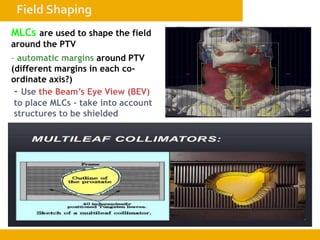
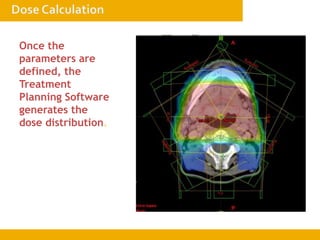
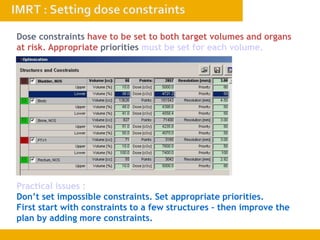
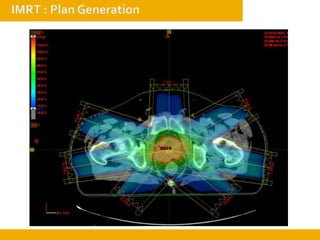
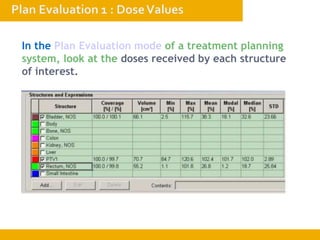
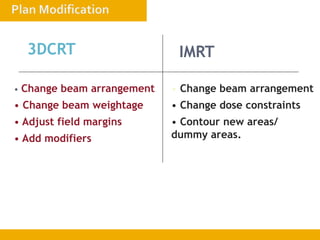
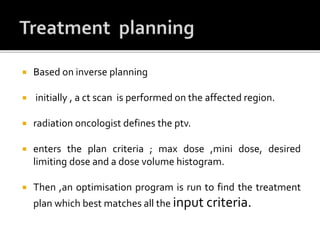
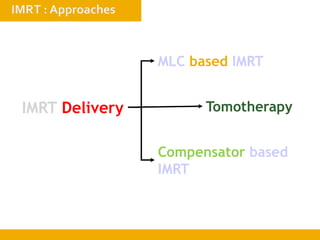
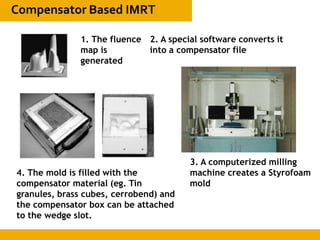
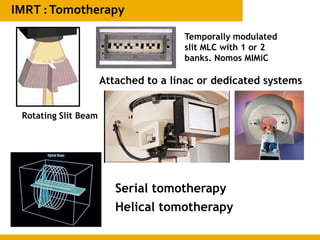
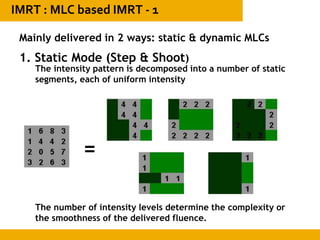
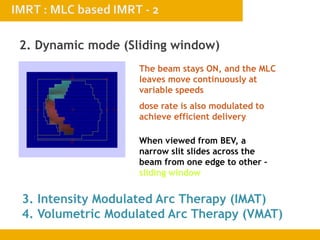
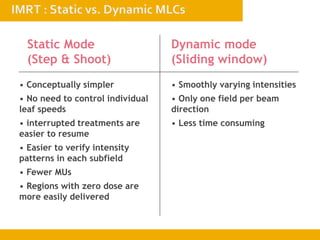
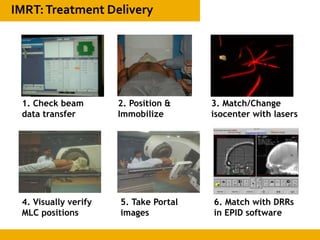
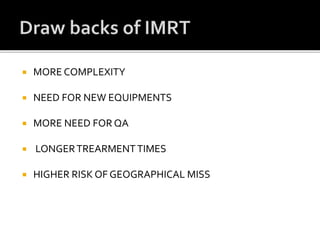
The document discusses intensity-modulated radiation therapy (IMRT), including its advantages over conventional radiation therapy in delivering higher and more uniform radiation doses to tumor volumes while minimizing doses to surrounding healthy tissues. It explains that IMRT uses computer-optimized inverse planning to calculate non-uniform radiation beam intensities that target the tumor from several angles. This allows complex tumor shapes to be more conformally treated with lower toxicity risks compared to conventional techniques.