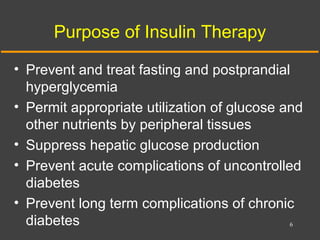
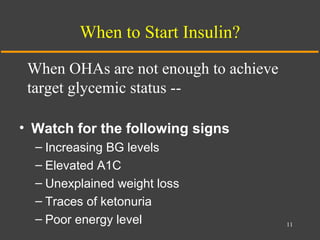
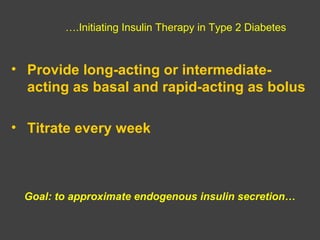
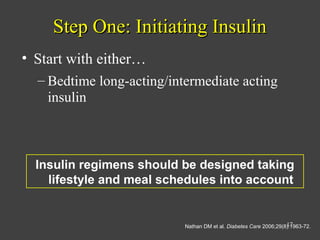
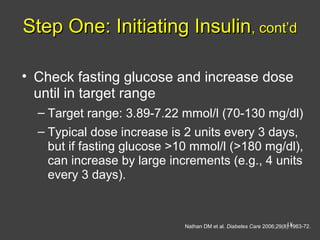
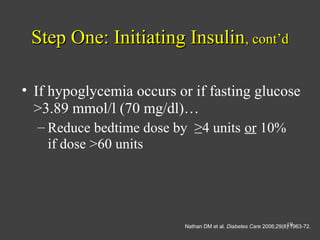
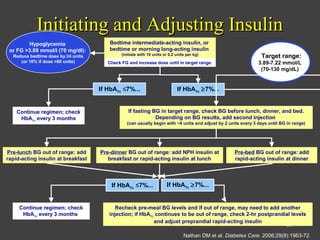
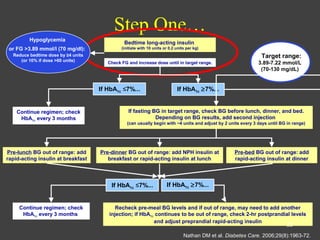
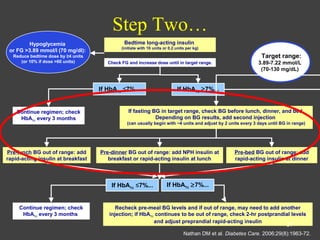
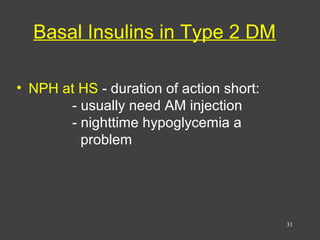
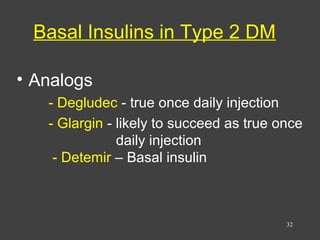
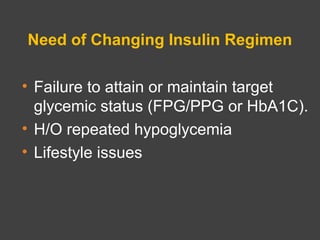
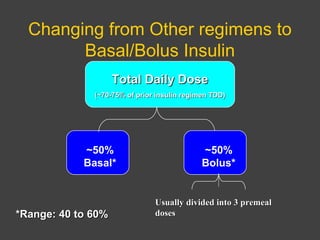
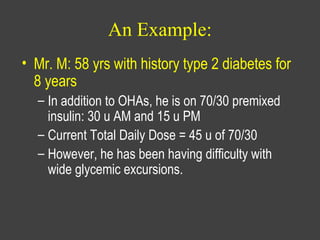
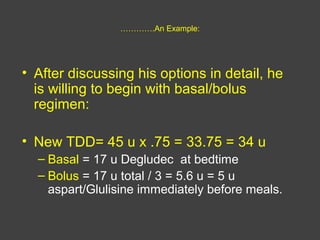
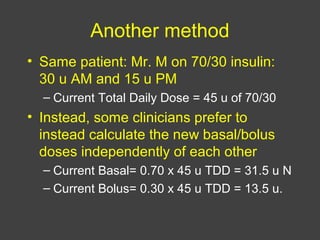
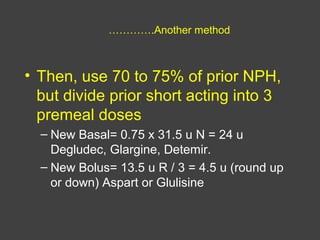
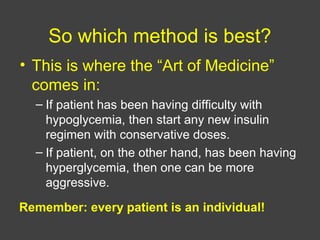
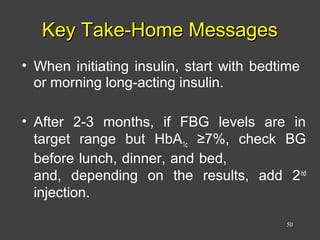
1) This document discusses the initiation and adjustment of insulin therapy for type 2 diabetes. It recommends starting with a long-acting basal insulin at bedtime and titrating the dose up gradually until fasting blood glucose is at target levels.
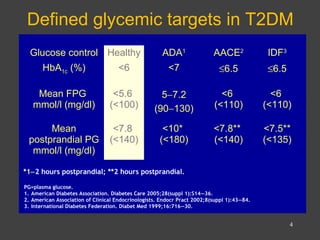
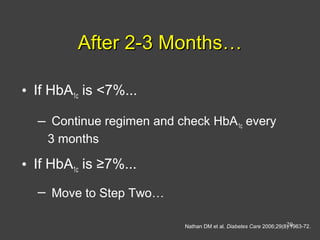
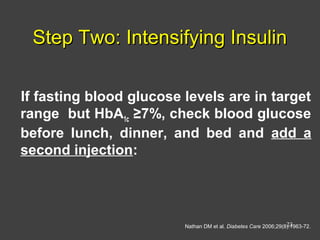
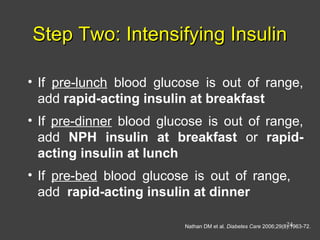
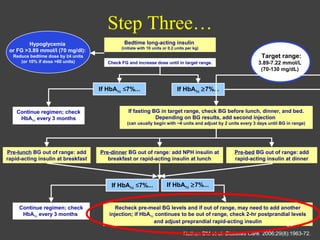
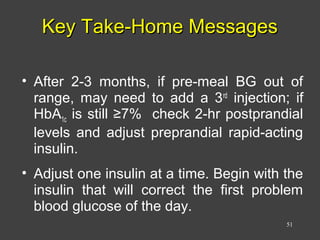
2) If HbA1c remains above 7% after 2-3 months, short-acting insulins should be added at mealtimes starting with breakfast. The doses are then titrated based on pre-meal blood glucose readings.
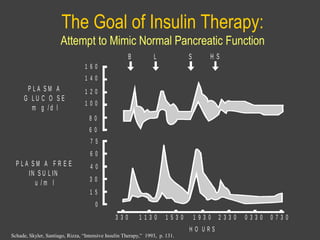
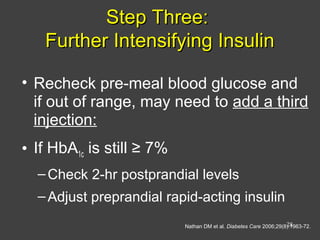
3) If HbA1c is still not at target after a further 2-3 months, a third daily insulin injection may be needed and post-meal blood glucose should be checked to guide adjustments. The goal is to approximate normal pancreatic