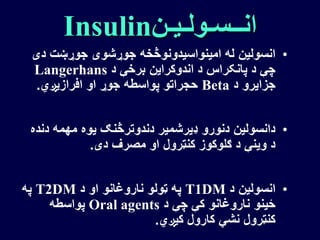
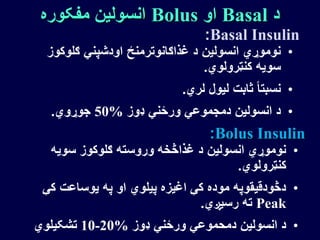
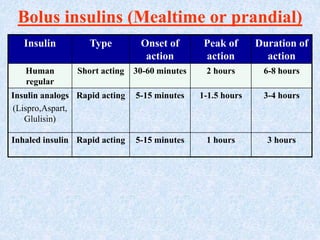
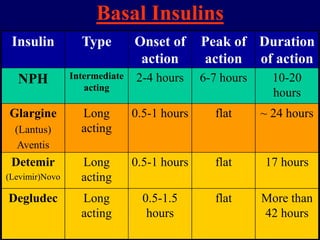
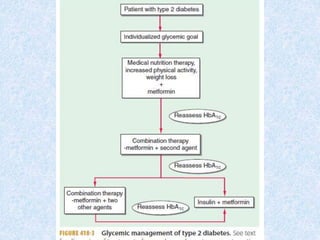
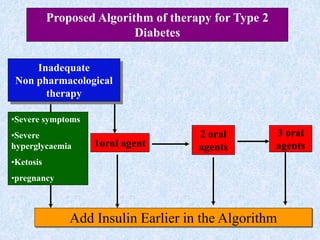
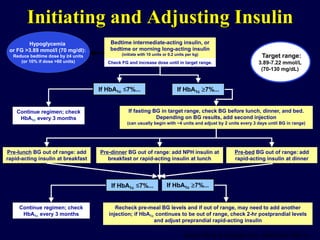
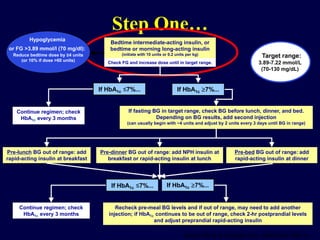
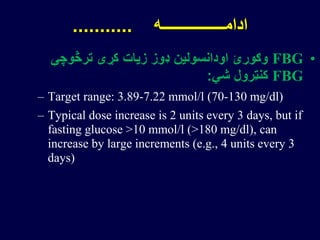
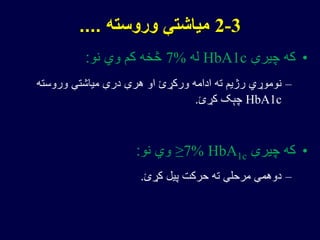
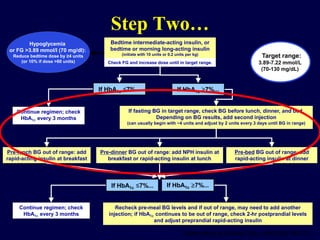
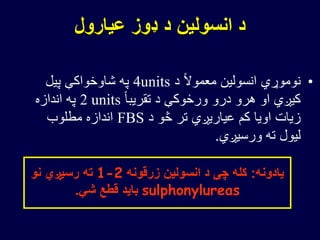
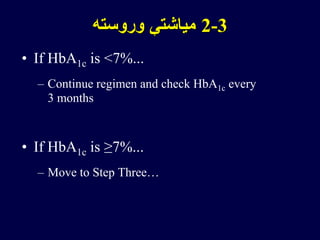
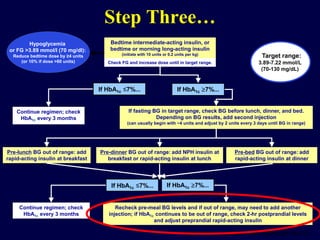
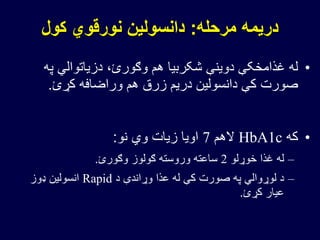
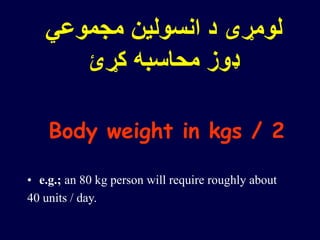
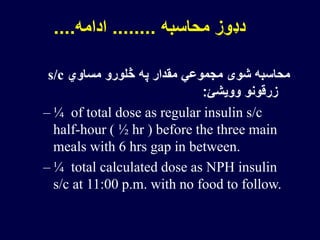
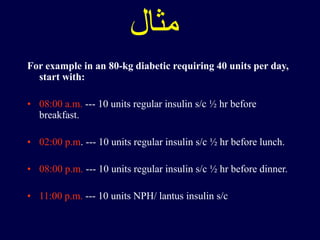
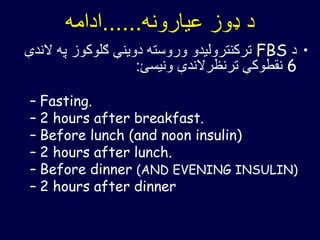
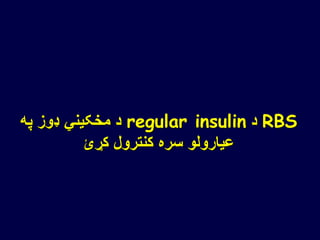
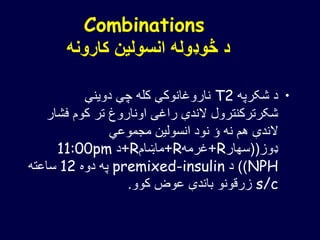
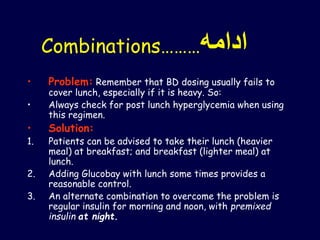
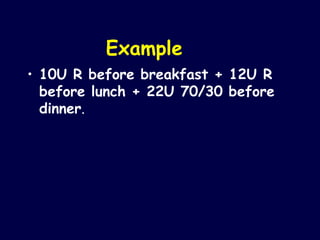
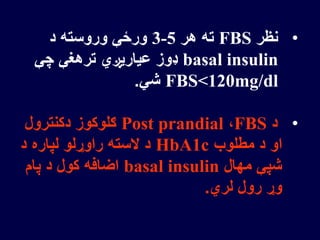
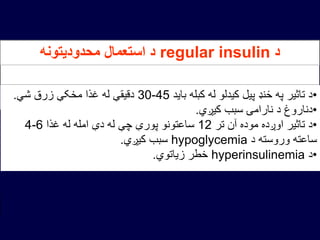
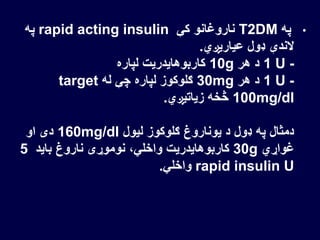
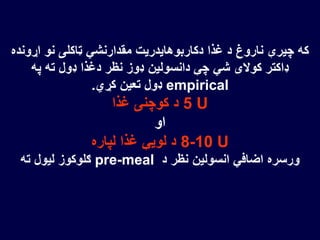
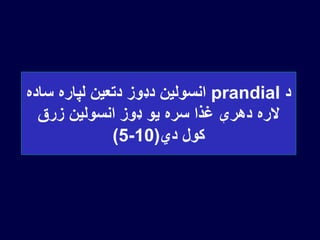
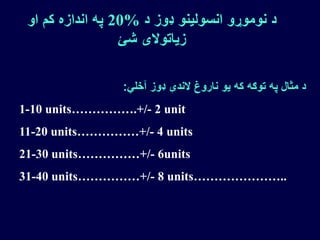
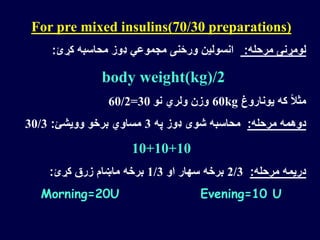
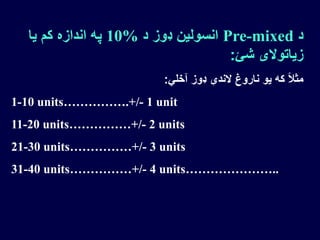
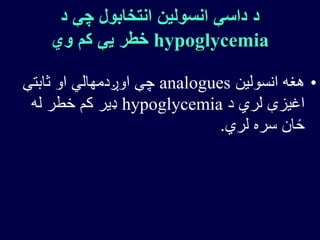
This document provides guidelines for initiating and adjusting insulin therapy for type 2 diabetes. It outlines a step-by-step regimen beginning with initiating either bedtime intermediate-acting insulin or bedtime or morning long-acting insulin. It instructs to monitor fasting blood glucose and increase the insulin dose until the target range is achieved. Additional injections of rapid-acting insulin are added before meals if blood glucose levels remain out of range. The regimen is monitored every 3 months by checking HbA1c and adjusting insulin doses up or down based on blood glucose levels and HbA1c targets.