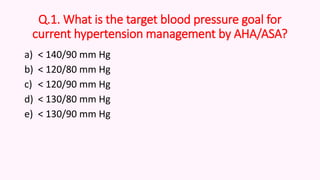
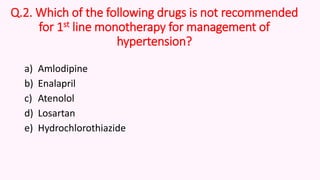
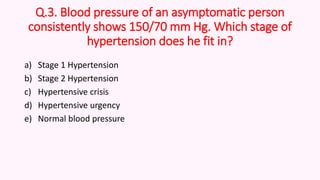
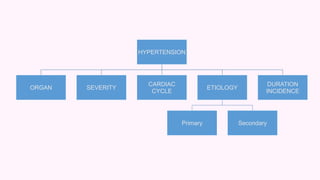
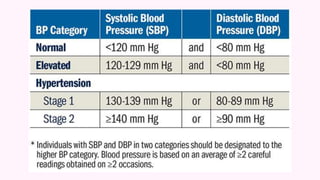
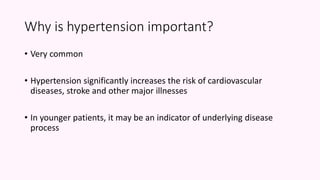
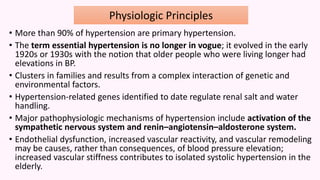
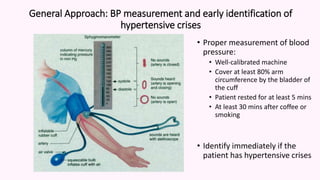
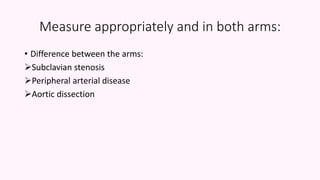
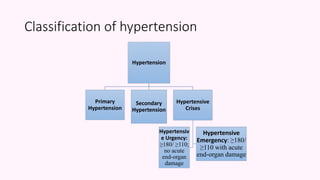
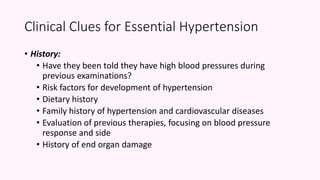
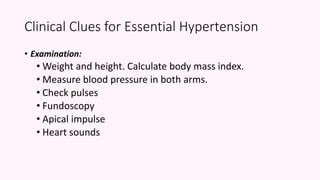
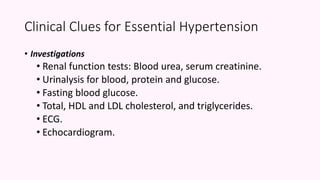
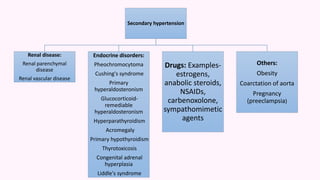
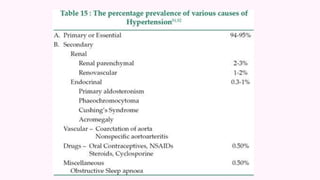
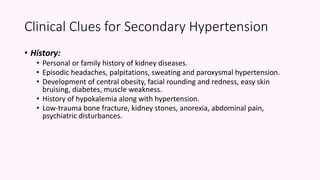
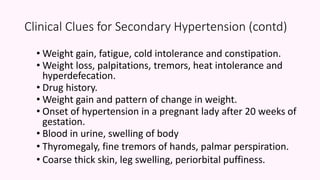
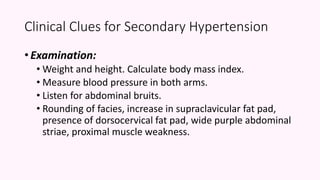
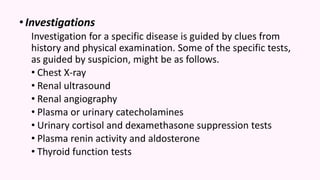
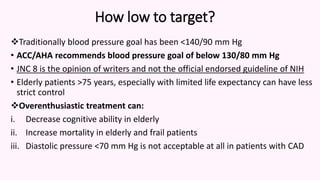
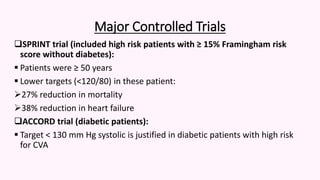
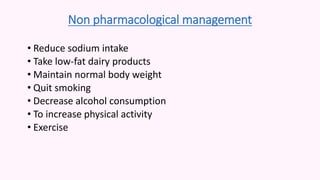
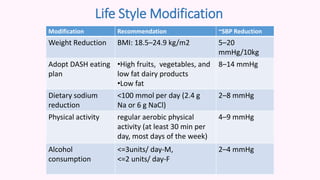
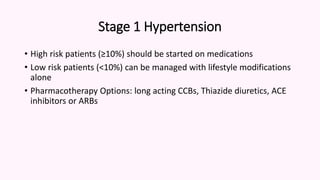
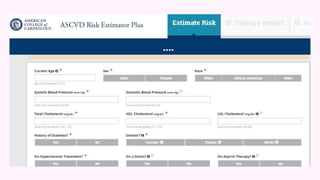
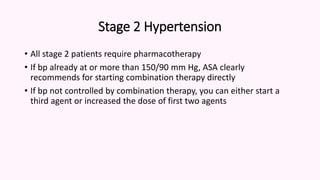
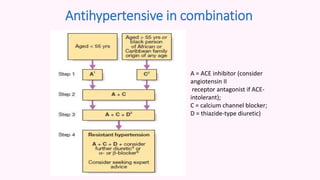
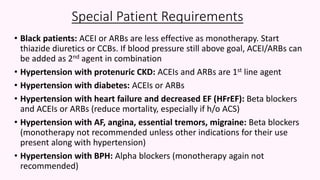
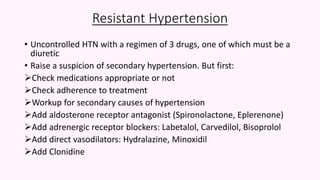
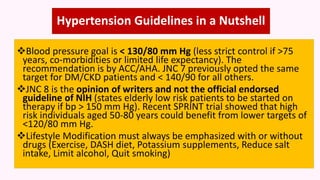
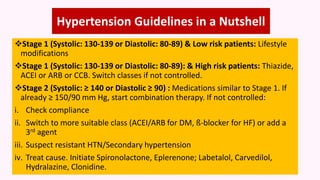
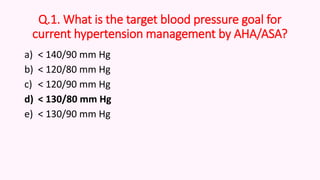
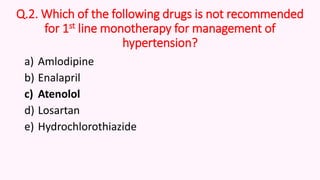
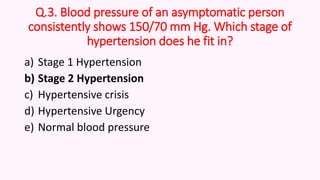
The document outlines guidelines for hypertension management, including recommended blood pressure targets and treatment options for different stages of hypertension. It emphasizes the importance of lifestyle modifications alongside pharmacotherapy, particularly for varying risk categories and specific patient needs. Additionally, it provides a review of clinical clues for primary and secondary hypertension and discusses the management of resistant cases.