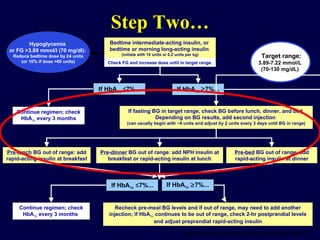
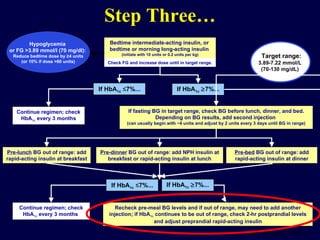
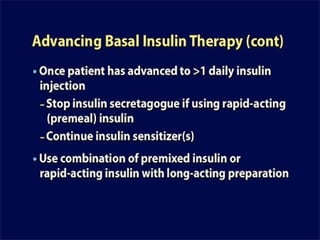
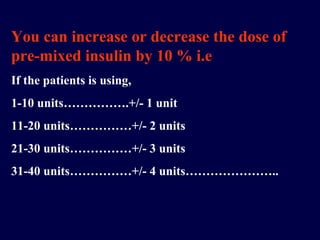
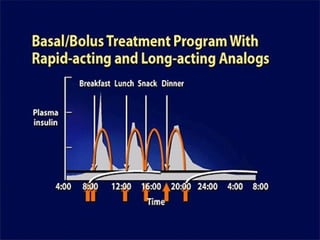
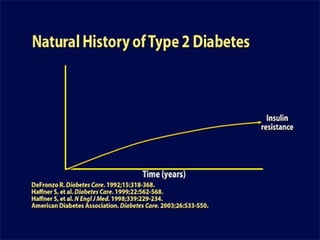
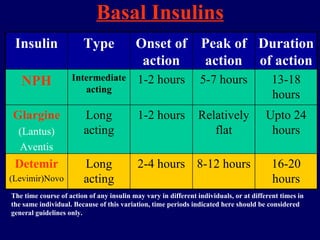
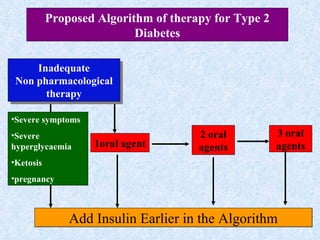
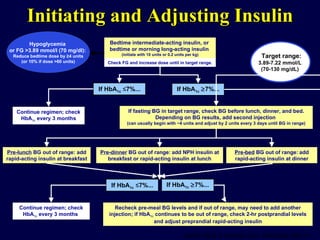
The document discusses guidelines for initiating insulin therapy in patients with type 2 diabetes not controlled on oral antidiabetic drugs (OADs). It recommends starting with either bedtime intermediate-acting insulin or bedtime or morning long-acting insulin, beginning at a dose of 10 units or 0.2 units/kg. The insulin dose is then titrated up based on fasting blood glucose levels until the target range is achieved. Additional injections of rapid-acting insulin may be added if pre-meal blood glucose levels remain out of range.





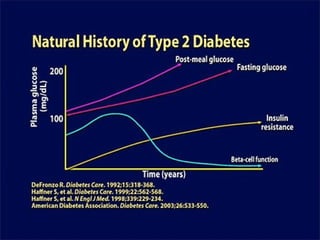












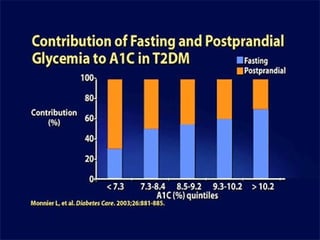




















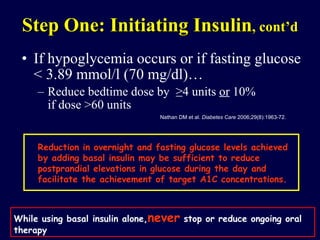

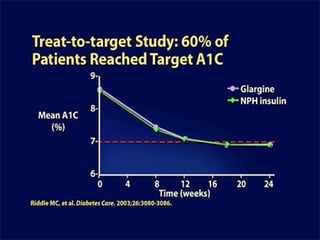
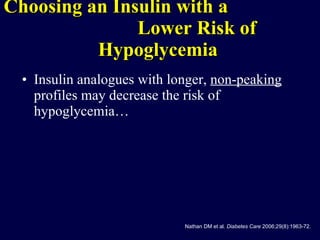
![With the addition of basal insulin and titration to target FBG levels, only about 60% of patients with type 2 diabetes are able to achieve A1C goals < 7%. [36] In the remaining patients with A1C levels above goal regardless of adequate fasting glucose levels, postprandial blood glucose levels are likely elevated.](https://image.slidesharecdn.com/insulintherapyindm-110209112727-phpapp02/85/Insulin-Therapy-in-DM-70-320.jpg)