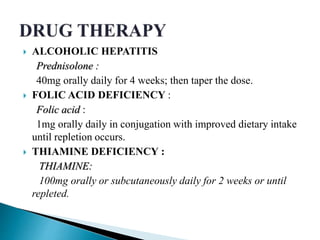
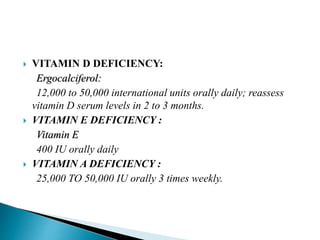
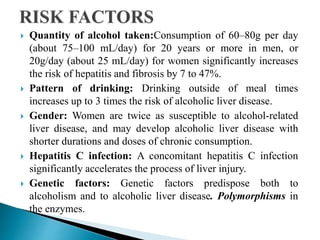
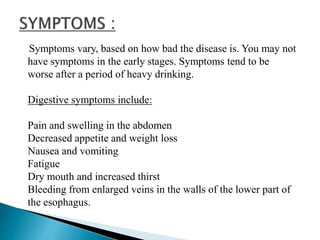
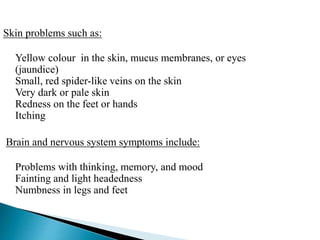
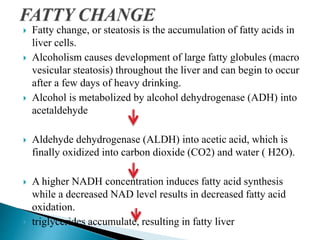
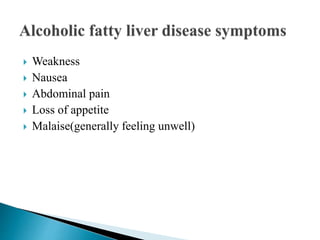
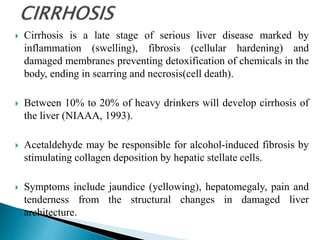
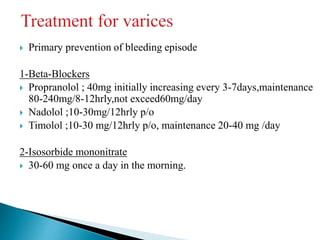
This document discusses alcoholic liver disease (ALD). It begins by defining ALD and its stages - fatty liver, alcoholic hepatitis, and cirrhosis. It then discusses risk factors like gender, genetics, and drinking patterns. Symptoms for each stage are provided. The pathophysiology of steatosis, hepatitis, and cirrhosis are explained. Diagnostic tests including blood tests, imaging, and biopsy are outlined. Management of ALD focuses on abstinence, nutrition, medications to prevent complications, and potentially transplantation for late-stage disease.
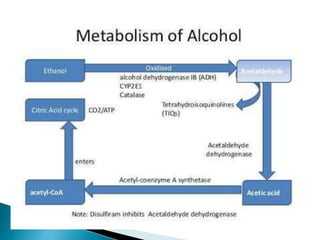
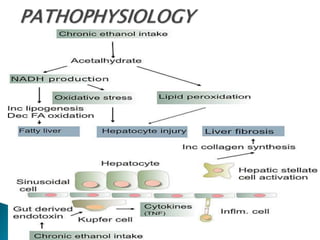
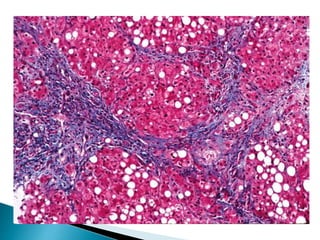
![ 80% of alcohol passes through the liver to be detoxified.
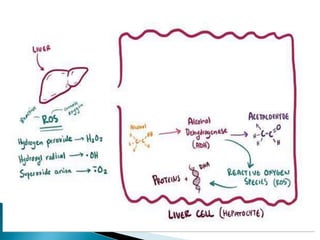
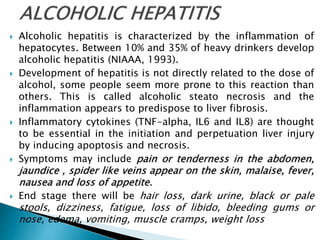
Chronic consumption of alcohol results in the secretion of pro-
inflammatory cytokines (TNF-alpha, Interleukin 6 [IL6] and
Interleukin 8 [IL8]), oxidative stress, lipid peroxidation, and
acetaldehyde toxicity.](https://image.slidesharecdn.com/ald-180226073505/85/Alcoholic-Liver-Disease-5-320.jpg)

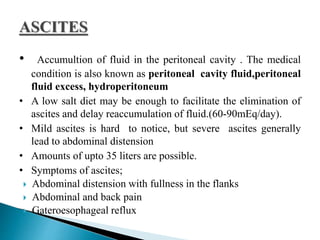

![Management of cirrhotic ascites
Bed rest and sodium restriction[60-90meq/day to
1500-2000mg of salt/day]
Spironolactone : 100-400 mg/day
Furosemide : 40-160mg/day
Hydrochlorothiazide : 50mg/day](https://image.slidesharecdn.com/ald-180226073505/85/Alcoholic-Liver-Disease-29-320.jpg)