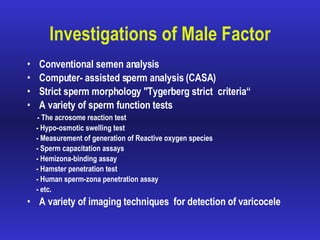
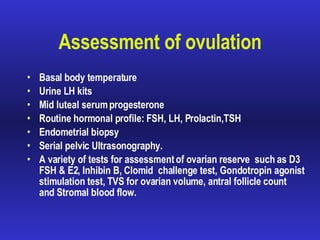
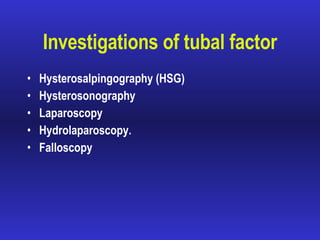
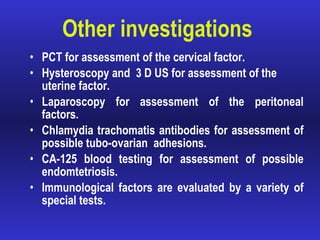
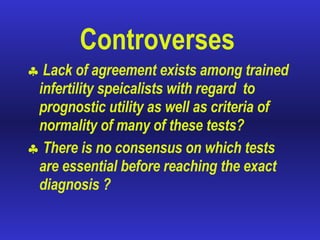
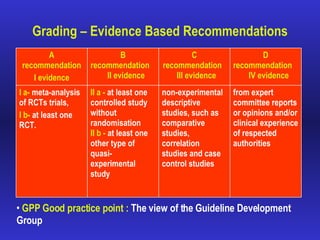
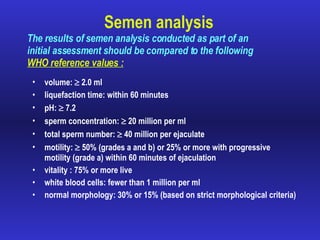
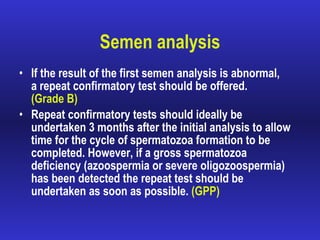
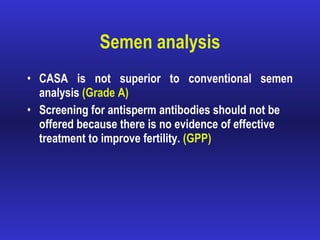
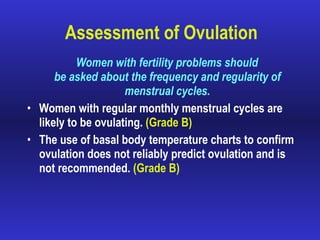
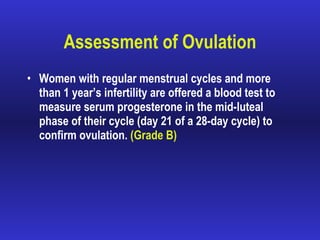
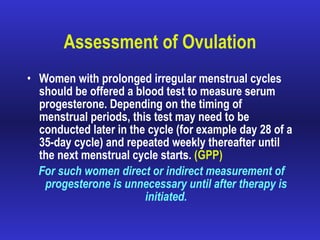
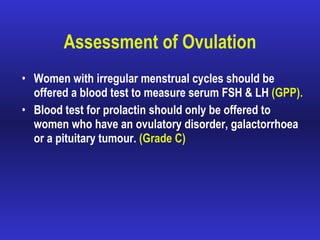
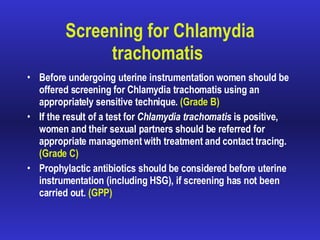
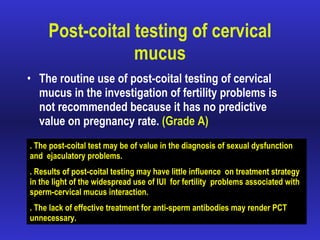
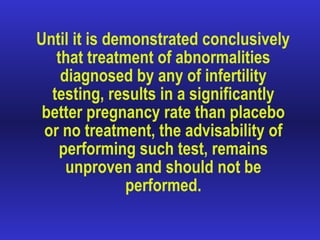
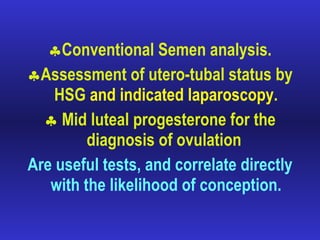
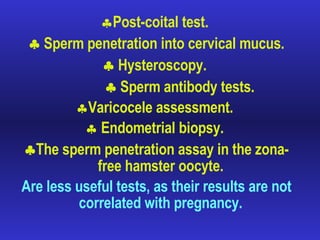
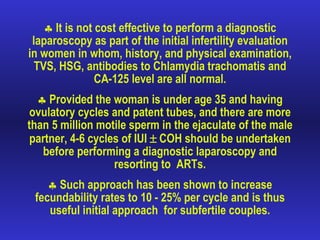
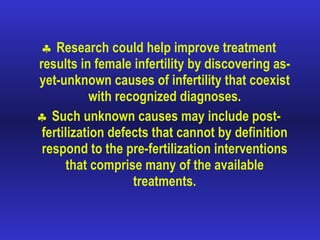
This document summarizes evidence-based guidelines for investigating infertile couples. It finds that while many tests have been advocated, the necessity and cost-effectiveness of many have not been proven. It recommends conventional semen analysis, assessment of ovulation with progesterone tests, and HSG or laparoscopy to assess tubal patency as useful initial tests. Tests like post-coital testing, hysteroscopy, and sperm penetration assays provide little predictive value on pregnancy rates and are less useful. A simplified approach focusing on proven essential tests can significantly reduce time and costs in evaluating infertility.