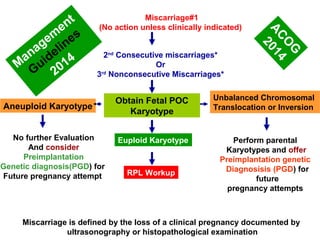
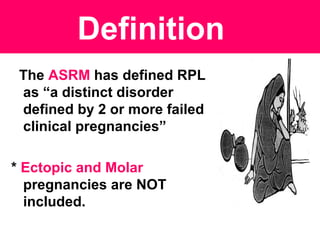
- Recurrent pregnancy loss is defined as 3 or more consecutive miscarriages before 20 weeks.
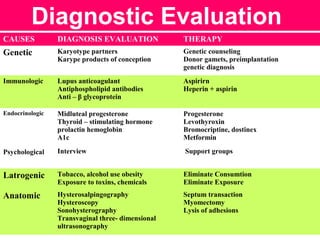
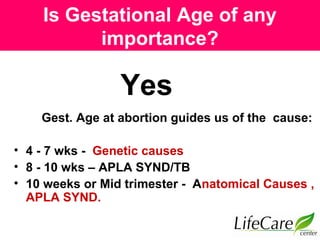
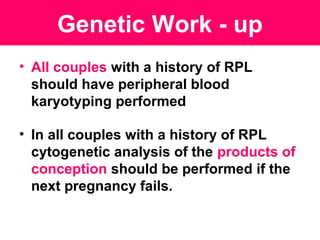
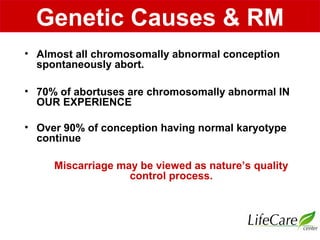
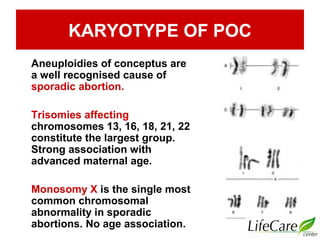
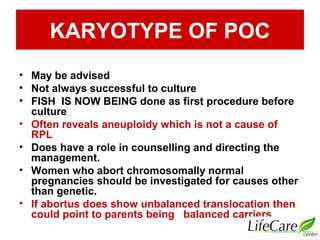
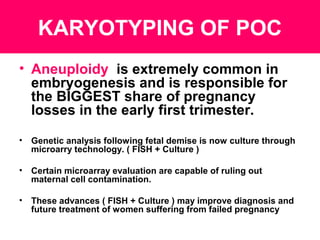
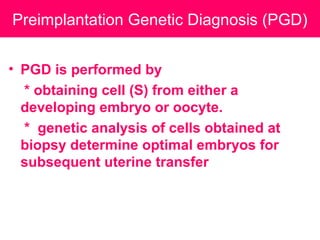
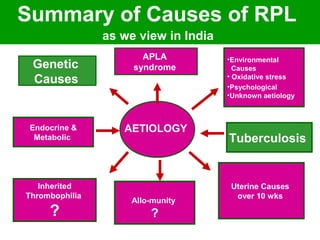
- Genetic causes like chromosomal abnormalities are a major cause and account for around 70% of early miscarriages. Karyotyping of pregnancy tissue can identify chromosomal abnormalities.
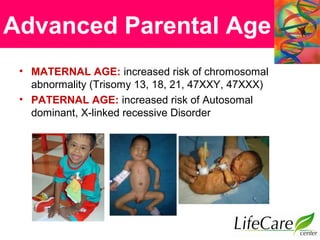
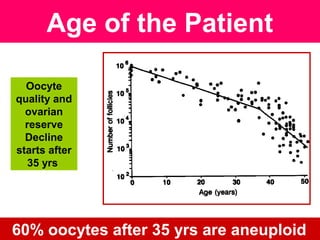
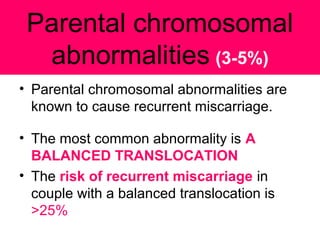
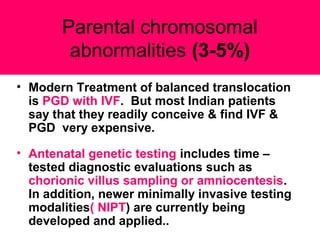
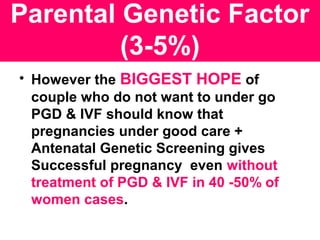
- Advanced parental age increases the risk of genetic defects leading to miscarriage due to declining egg/sperm quality. Parental karyotyping may identify balanced translocations in 3-5% of couples.
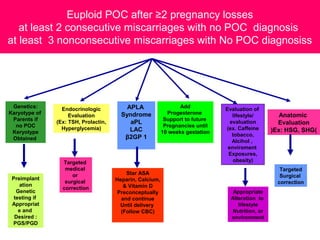
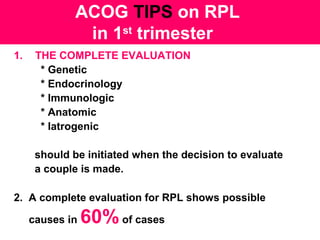
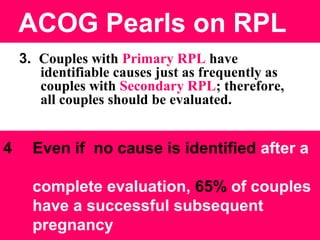
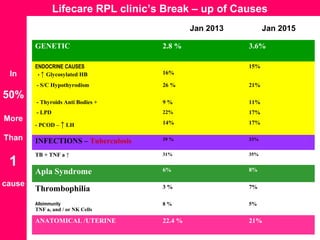
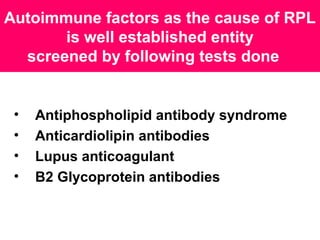
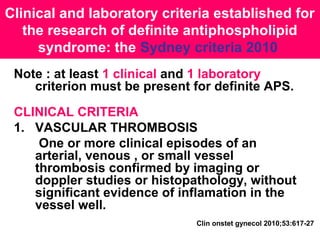
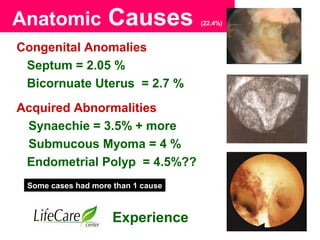
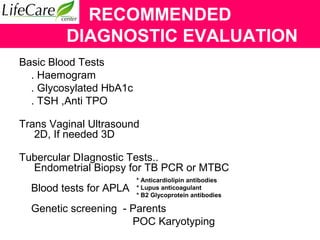
- A thorough evaluation including genetic, endocrine, anatomical, immunological, and infectious factors can identify a cause in 60% of recurrent pregnancy loss cases.




![Unexplained R.P.L.
In 40% of R.P.L. cases - cause remains
undetermined
While recent research work has focused On
• TUBERCULAR ENDOMETRITIS [INDIAN
DOCTORS]
• Thrombophilia
• Spermatozoal
• Embryonic
• Endometrial characteristics
Last Word is Still Missing !](https://image.slidesharecdn.com/anupdateonrecurrentpregnancyloss2015-150214010640-conversion-gate01/85/An-update-on-recurrent-pregnancy-loss-2015-14-320.jpg)