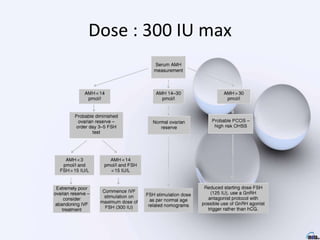
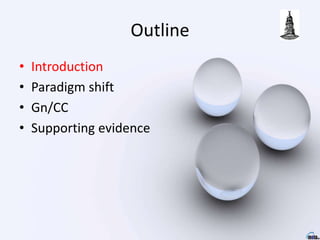
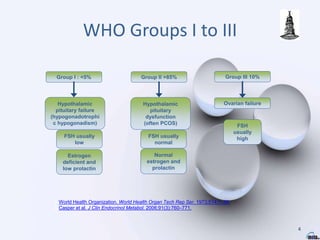
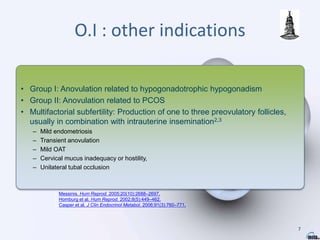
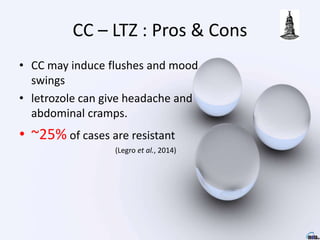
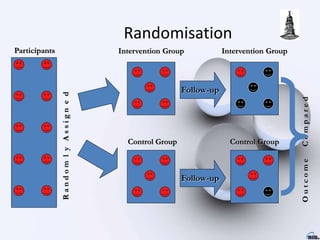
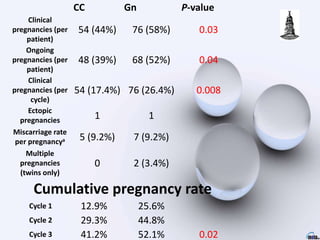
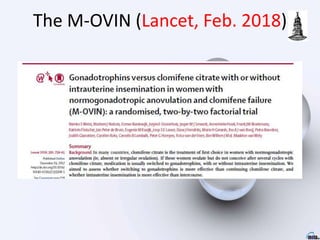
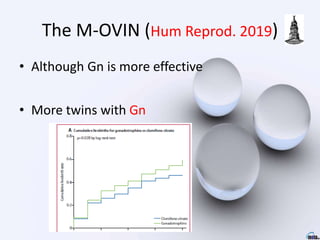
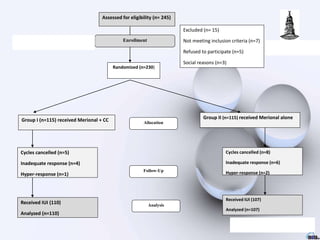
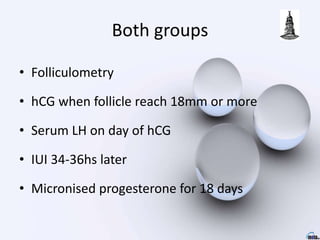
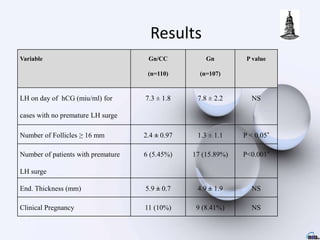
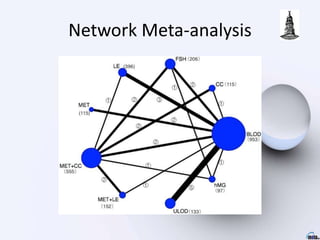
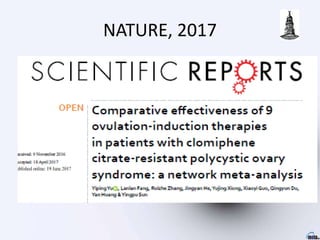
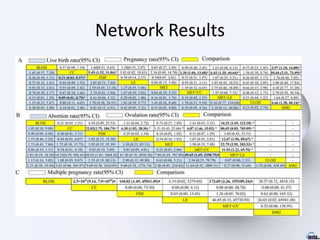
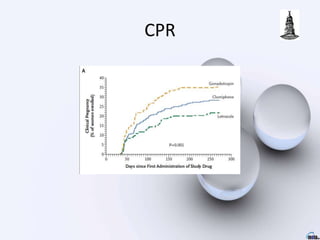
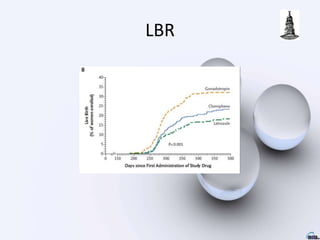
The document provides an update on ovulation stimulation, discussing the need for evidence-based treatments for infertility, particularly for patients with conditions such as PCOS and hypogonadotrophic hypogonadism. It outlines various treatment groups, compares the efficacy of different drugs like clomiphene citrate and gonadotropins, and highlights a recent study that shows gonadotropins lead to higher pregnancy rates than clomiphene citrate. Additionally, it emphasizes the importance of considering cost-effectiveness when choosing treatment options for patients.


![666 Women
• Gn group had more livebirths than CC
• [52%] vs [41%] p=0·012
• Addition of IUI did not increase
livebirths compared with intercourse
p=0·11](https://image.slidesharecdn.com/o-211112090752/85/O-i-2021-16-320.jpg)







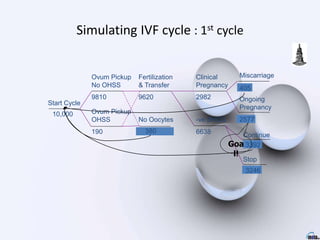
![Miscarriage
p_miscar_rFSH
Start Cycle
Pregnancy
#
Ongoing Pregnancy
Clinical Pregnancy
p_clin_preg_rFSH
continue
#
Start Cycle
stop
t_discon_nomed[ _stage]
Stop IVF
-ve bHCG
#
Fertilization &
Embryo Transfer
#
No Oocytes
p_cancel_rFSH
Start Cycle
Ovum Pickup
No OHSS
#
Miscarriage
p_miscar_rFSH
Start Cycle
Pregnancy
#
Ongoing Pregnancy
Clinical Pregnancy
p_clin_preg_rFSH
continue
#
Start Cycle
stop
t_discon_nomed[ _stage]
Stop IVF
-ve bHCG
#
Fertilization &
Embryo Transfer
#
No Oocytes
p_cancel_rFSH
Start Cycle
Ovum Pickup
OHSS
p_OHSS_rFSH
Start Cycle
1
Ongoing Pregnancy
0
Stop IVF
0
rFSH
Miscarriage
p_miscar_hMG
Start Cycle
Pregnancy
#
Ongoing Pregnancy
Clinical Pregnancy
p_clin_preg_hMG
continue
#
Start Cycle
stop
t_discon_nomed[ _stage]
Stop IVF
-ve bHCG
#
Fertilization &
Embryo Transfer
#
No Oocytes
p_cancel_hMG
Start Cycle
Ovum Pickup
No OHSS
#
Miscarriage
p_miscar_hMG
Start Cycle
Pregnancy
#
Ongoing Pregnancy
Clinical Pregnancy
p_clin_preg_hMG
continue
#
Start Cycle
stop
t_discon_nomed[ _stage]
Stop IVF
-ve bHCG
#
Fertilization &
Embryo Transfer
#
No Oocytes
p_cancel_hMG
Start Cycle
Ovum Pickup
OHSS
p_OHSS_hMG
Start Cycle
1
Ongoing Pregnancy
0
Stop IVF
0
hMG
Ovarian
Stimulant](https://image.slidesharecdn.com/o-211112090752/85/O-i-2021-67-320.jpg)