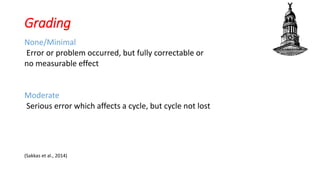
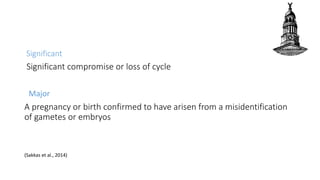
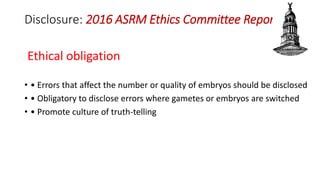
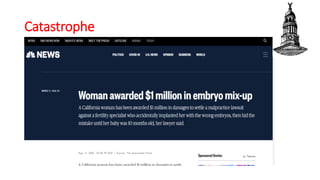
The document discusses the management of errors that can occur during the IVF process, categorizing them into clinical, administrative, and embryo lab errors. It outlines strategies to avoid such errors, including proper staffing, training, and procedural protocols, as well as the importance of transparency and disclosure to patients about any incidents. Grading of errors is provided to assess their impact on treatment cycles, emphasizing the need for a culture of truth-telling in medical practice.