This document discusses infective endocarditis (IE), including:
- IE is caused by microbial infection of the heart endothelium or foreign bodies like prosthetic valves. It is life-threatening but uncommon. Morbidity and mortality remain high despite advances.
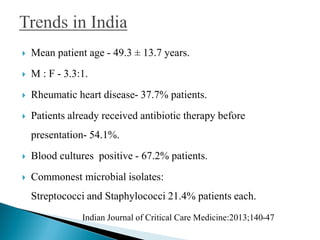
- Incidence is estimated at 1.7-6.2 per 100,000 patient-years in Western countries and 17,000 cases per year in India, often affecting younger patients with rheumatic or congenital heart disease.
- Staphylococcus aureus is the most common cause in developed nations while viridans group streptococci are common in developing countries. Multidrug resistance is a growing problem.
- Diagnosis



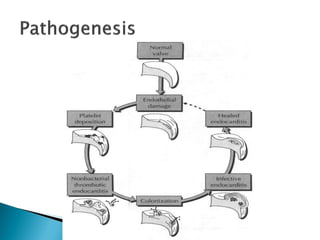

![ Also occur as a consequence of chewing and tooth brushing.
Such spontaneous bacteraemia - low grade and short duration
[1– 100 cfu/ml of blood for 10 min]
Both magnitude of bacteraemia and ability of the pathogen to
attach to damaged valves are important
Its high incidence explain why most cases of IE are unrelated
to invasive procedures.
Ann Intern Med 1998;129: 761–769.](https://image.slidesharecdn.com/infectiveendocarditispdf-170803082335/85/Infective-endocarditis-pdf-6-320.jpg)