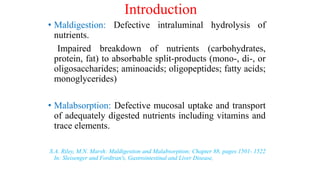
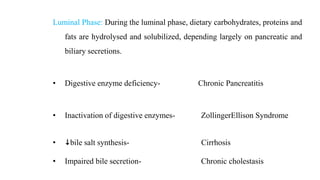
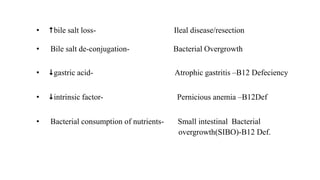
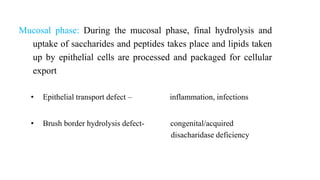
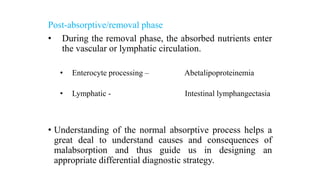
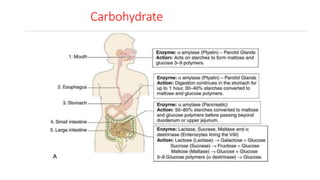
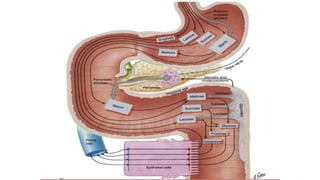
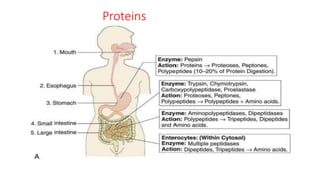
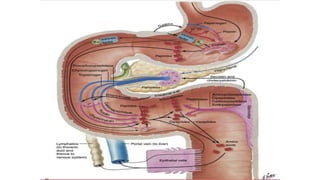
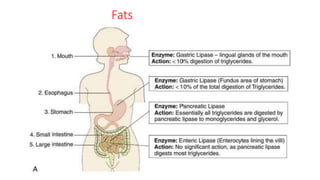
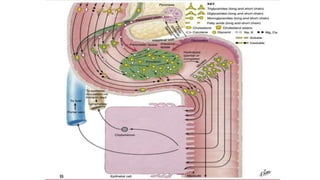
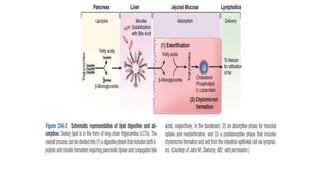
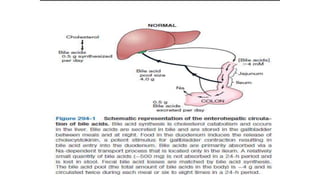
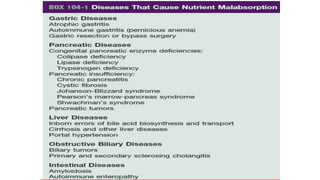
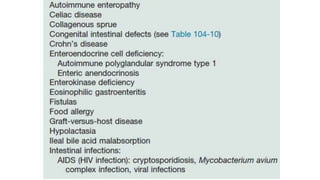
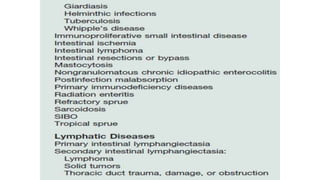
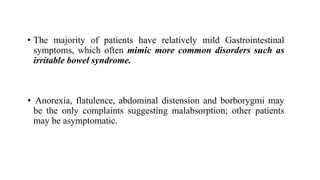
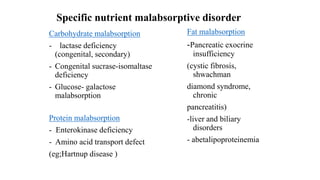
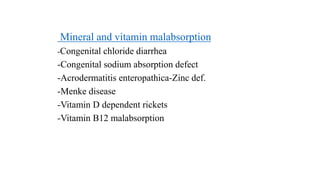
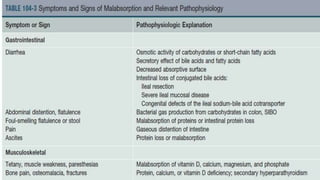
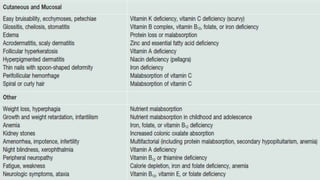
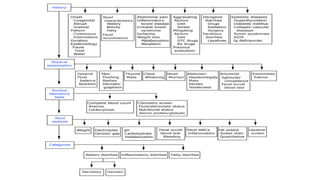
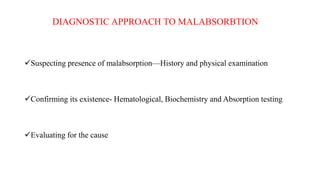
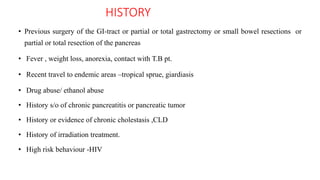
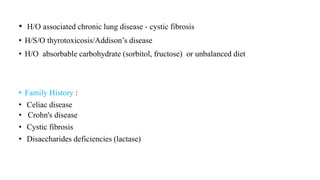
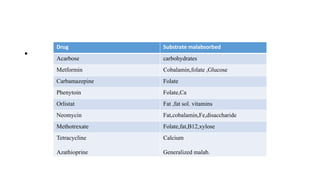
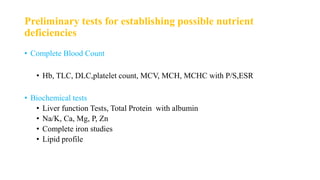
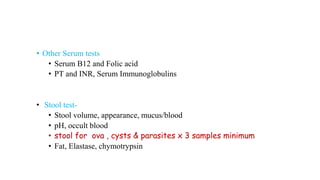
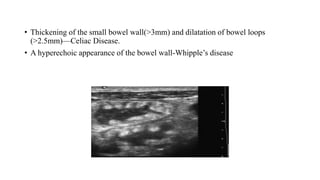
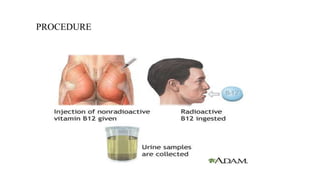
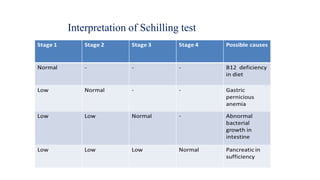
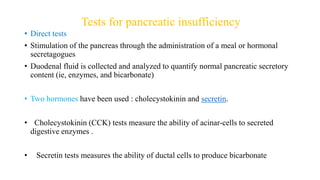
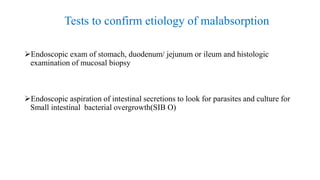
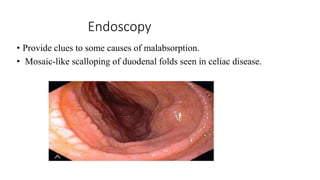
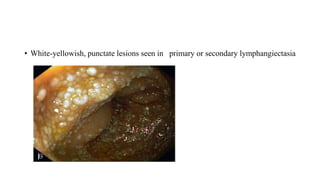
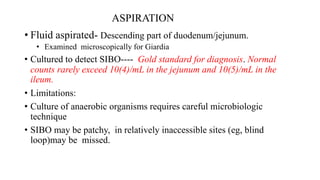
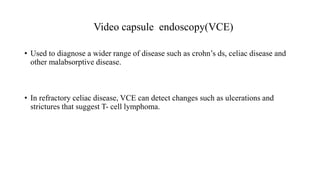
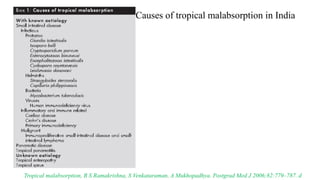
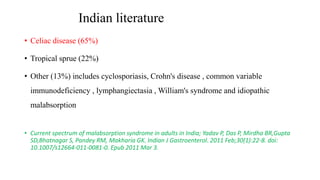
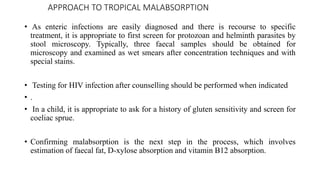
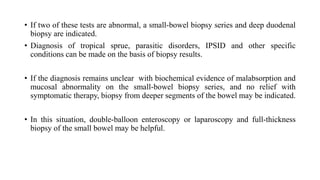
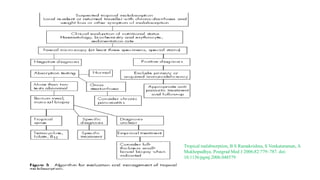
This document provides an overview of the approach to malabsorption syndrome. It discusses the mechanisms of malabsorption including defects that can occur in the luminal, mucosal, and post-absorptive phases. It describes specific causes of carbohydrate, protein, and fat malabsorption. Clinical manifestations can range from severe steatorrhea and weight loss to subtle changes on labs. The diagnostic approach involves considering malabsorption based on history and physical, confirming with hematological and biochemical tests, and evaluating the underlying cause with tests like imaging, endoscopy, and nutrient absorption tests.