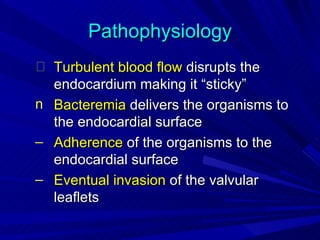
1. Infective endocarditis is an infection of the heart valves or endocardium. It can affect native or prosthetic valves.
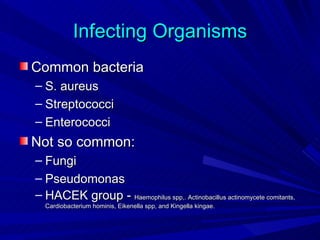
2. Risk factors include artificial heart valves, congenital heart defects, and intravenous drug use. Common causative organisms are staphylococci and streptococci.
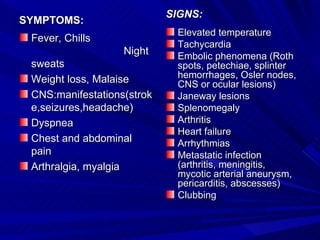
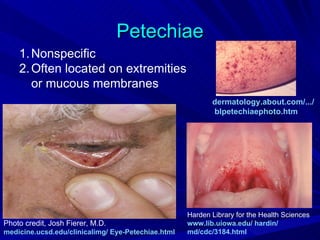
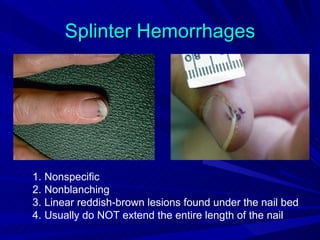
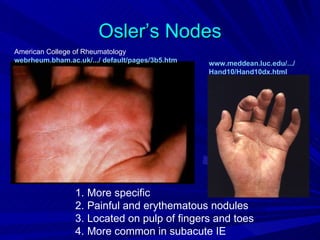
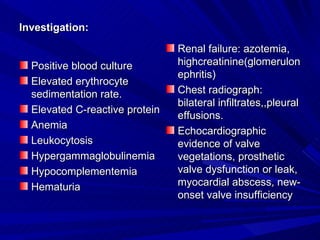
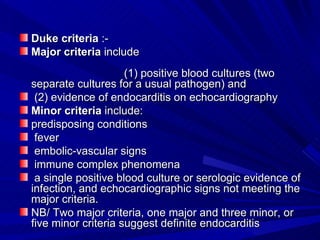
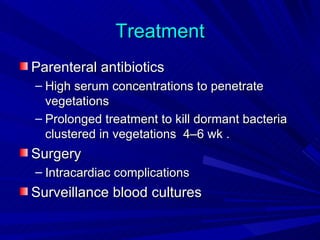
3. Symptoms include fever, chills, weight loss, and heart failure. Signs include heart murmurs, petechiae, splinter hemorrhages, and Osler's nodes. Diagnosis involves blood cultures and echocardiography. Treatment is intravenous antibiotics for 4-6 weeks along with possible surgery.