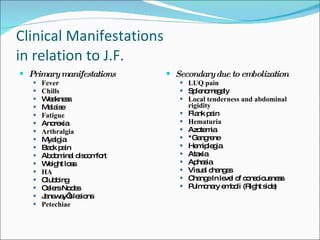
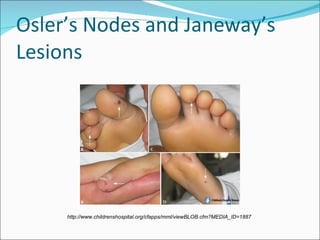
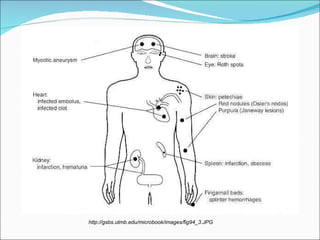
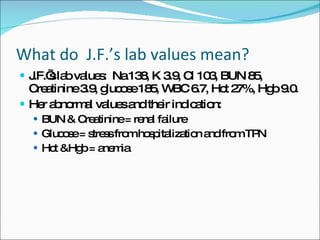
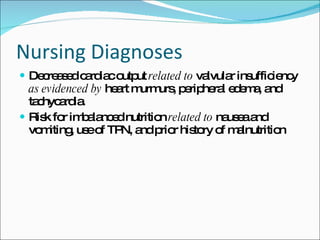
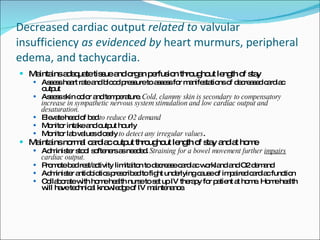
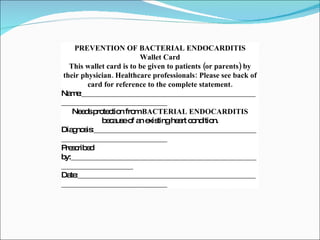
J.F. is a 50-year-old woman admitted with recurrent endocarditis, nausea, vomiting and renal failure. She has a history of autoimmune deficiency, heart valve infections, malnutrition and heart issues. On admission, she has signs of decreased cardiac output like edema and murmurs. Lab results show renal failure and anemia. She requires long-term IV antibiotics and nutrition support to treat her current endocarditis infection and underlying conditions.