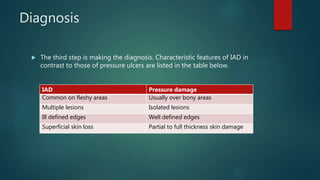
This document defines incontinence-associated dermatitis (IAD) as inflammation and skin breakdown caused by contact with urine or feces. It describes the skin's structure and functions, and explains that IAD occurs when constant contact with urine and feces disrupts the skin's barrier and natural pH. Predisposing factors include age, medications, mobility issues, and improper hygiene. Diagnosis involves skin assessment to differentiate IAD from pressure ulcers. Treatment focuses on cleansing after incontinence, applying effective skin barriers, and monitoring progress with emollients as needed.