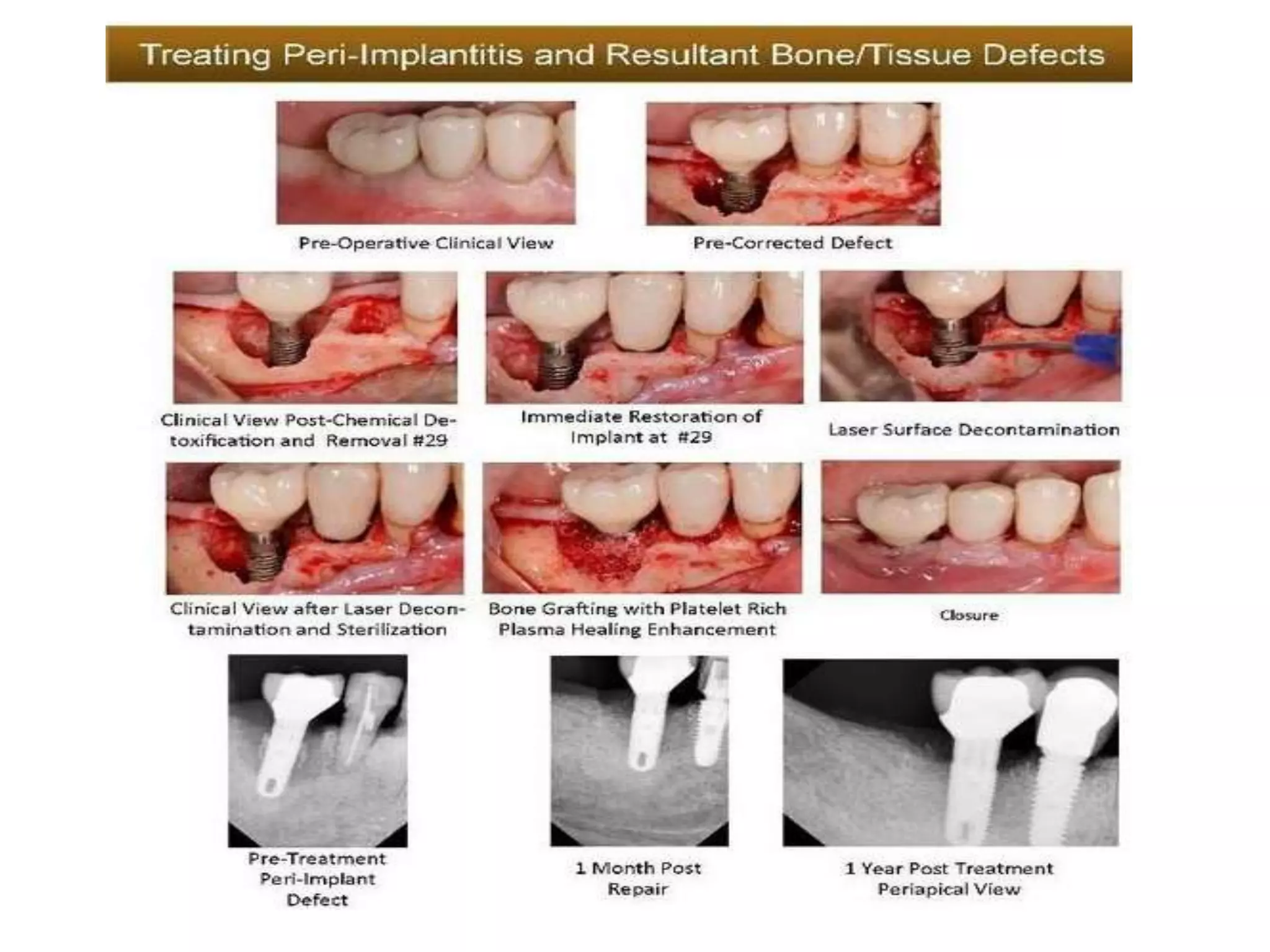
Periodic maintenance of dental implants through professional cleanings and home care is vital for long-term success. Maintenance visits should occur every 3 months for the first year, then adjust based on the patient's needs. Evaluations include examining soft tissues, bone levels on x-rays, implant stability, home care, and making any necessary repairs. Treatment for peri-implant mucositis is nonsurgical cleaning, while peri-implantitis may require surgery to treat bone loss. Proper maintenance protects implant function over many years.