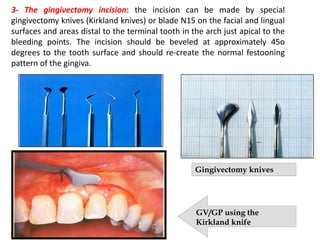
Gingival enlargement refers to excessive overgrowth of gum tissue surrounding teeth. It has several potential causes including inflammation, medications, and certain medical conditions. Treatment involves first managing any inflammatory component, and then surgical procedures such as gingivectomy or gingivoplasty may be performed to reshape the gums. These procedures aim to eliminate pockets and establish a healthy gum contour, but can result in loss of gum tissue or recession. Crown lengthening is a related procedure to increase the amount of visible tooth structure and is used for restorative or aesthetic reasons. It may involve gingivectomy, osseous recontouring, or repositioning of gum tissue. Maintaining an adequate biologic width between restoration