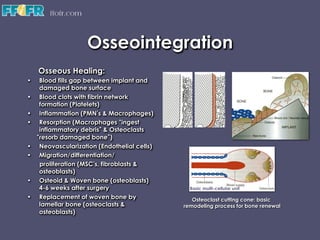
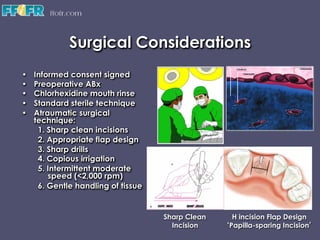
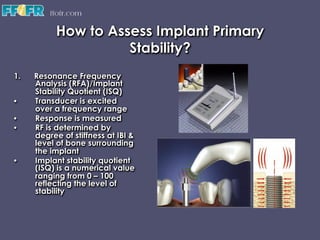
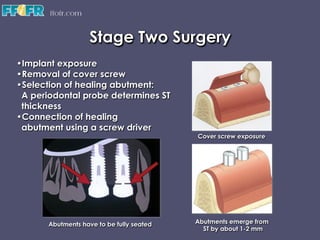
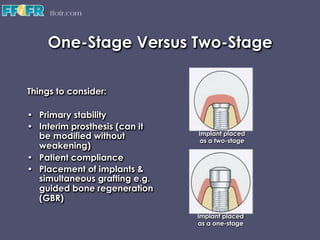
This document summarizes key aspects of dental implant surgery including osseointegration, surgical considerations, anatomical considerations, implant stability assessment, one-stage versus two-stage surgery, and extraction and immediate implant placement. It discusses the direct bone-implant connection called osseointegration, factors that influence osseous healing like implant surface characteristics, and techniques for ensuring primary stability. Key anatomical structures like nerves and sinuses are reviewed for surgical safety. Methods of evaluating initial implant stability like resonance frequency analysis are presented. The document compares one-stage and two-stage surgical protocols and reviews when immediate placement is appropriate.