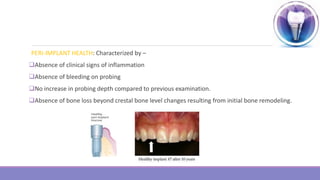
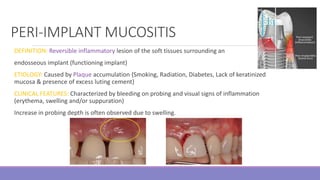
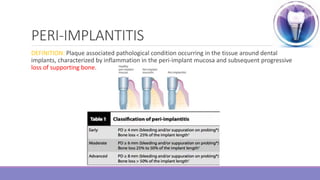
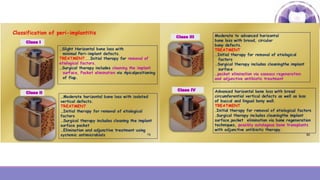
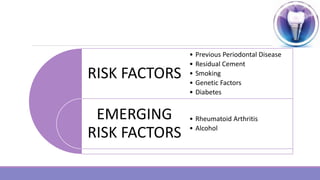
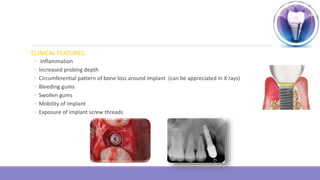
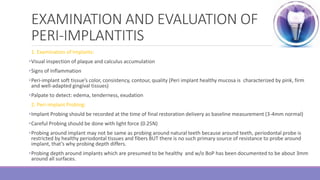
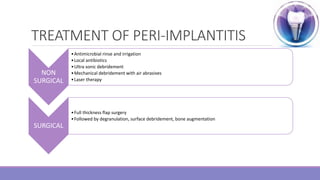
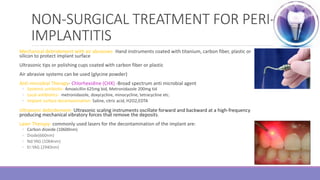
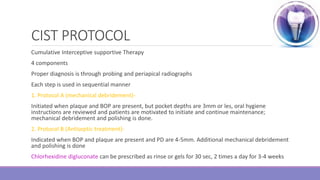
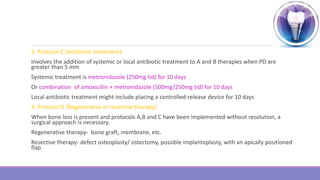
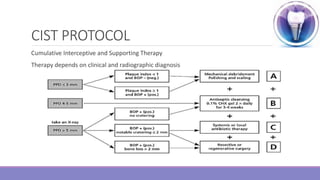
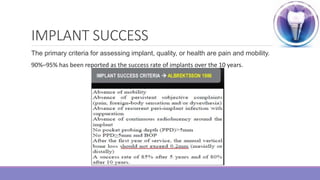
Peri-implantitis is a pathological inflammatory condition affecting the tissues surrounding dental implants, characterized by inflammation of the peri-implant mucosa and progressive bone loss. It is caused by plaque accumulation on the implant surface. Risk factors include a history of periodontitis and smoking. Treatment involves non-surgical mechanical debridement using air abrasives or ultrasonic tips for mild cases. More severe cases may require surgical debridement and decontamination of the implant surface along with local or systemic antibiotics. Long-term maintenance therapy and adherence to the CIST protocol are important for managing peri-implantitis and ensuring the success of dental implants.