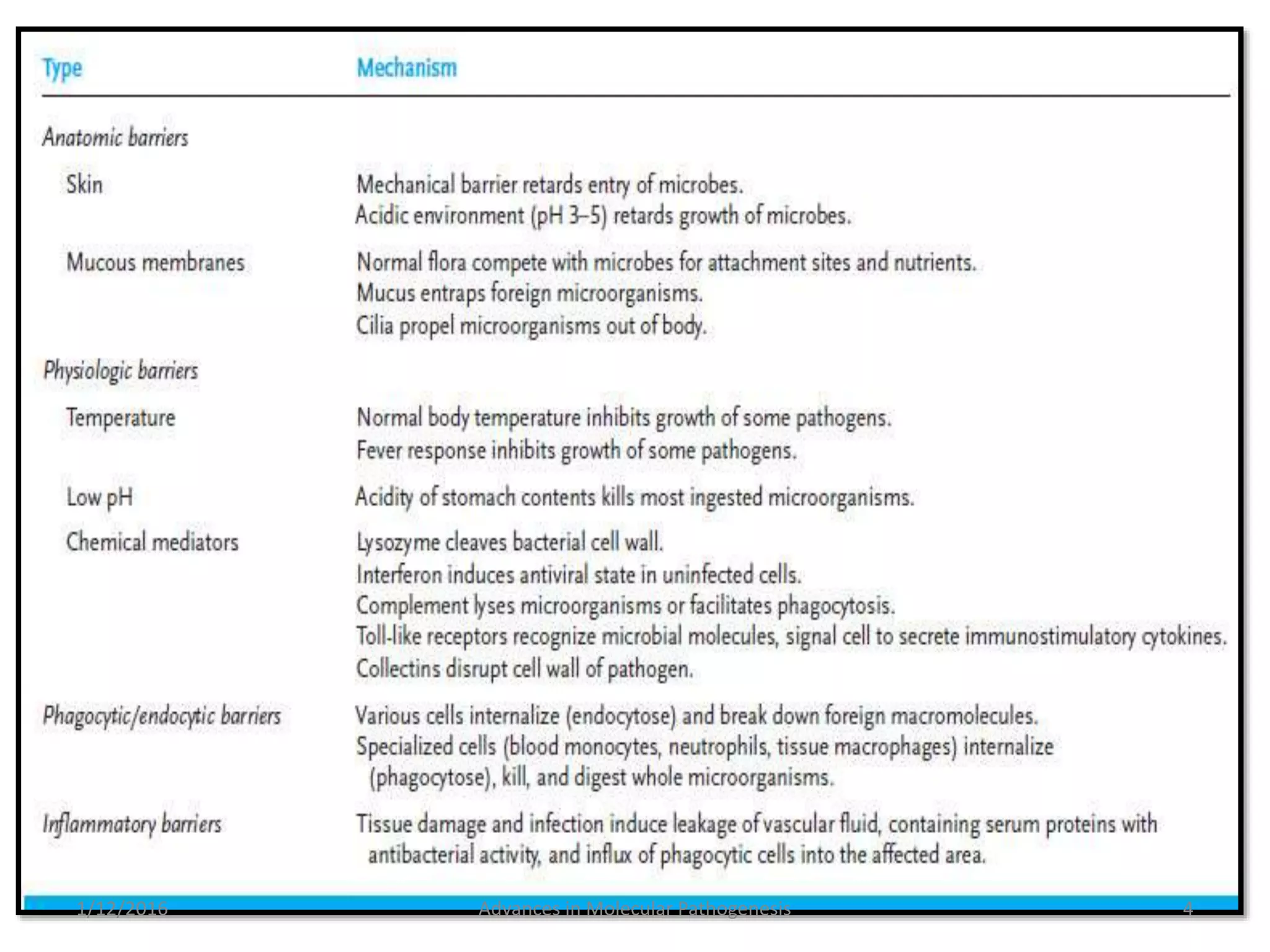
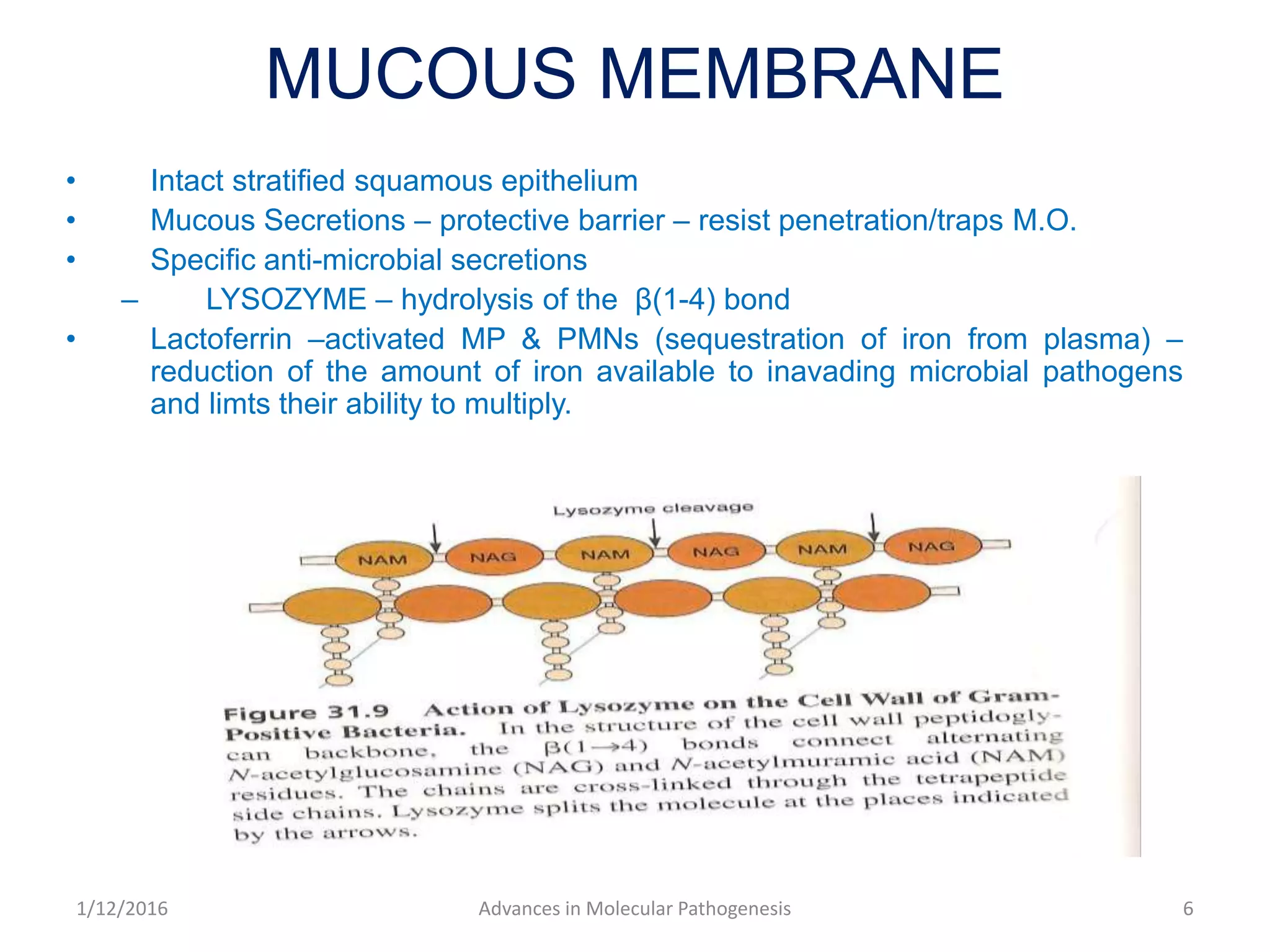
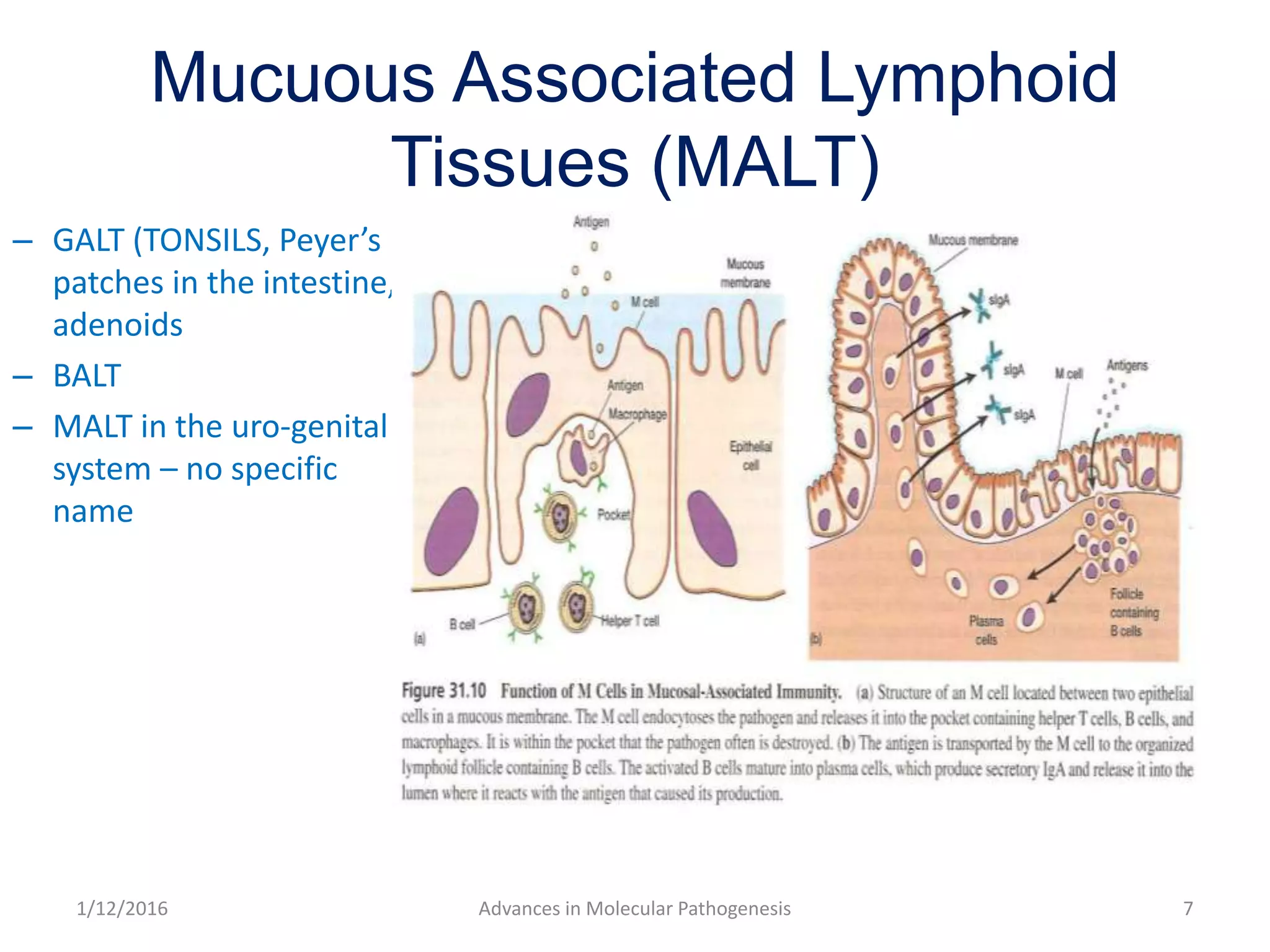
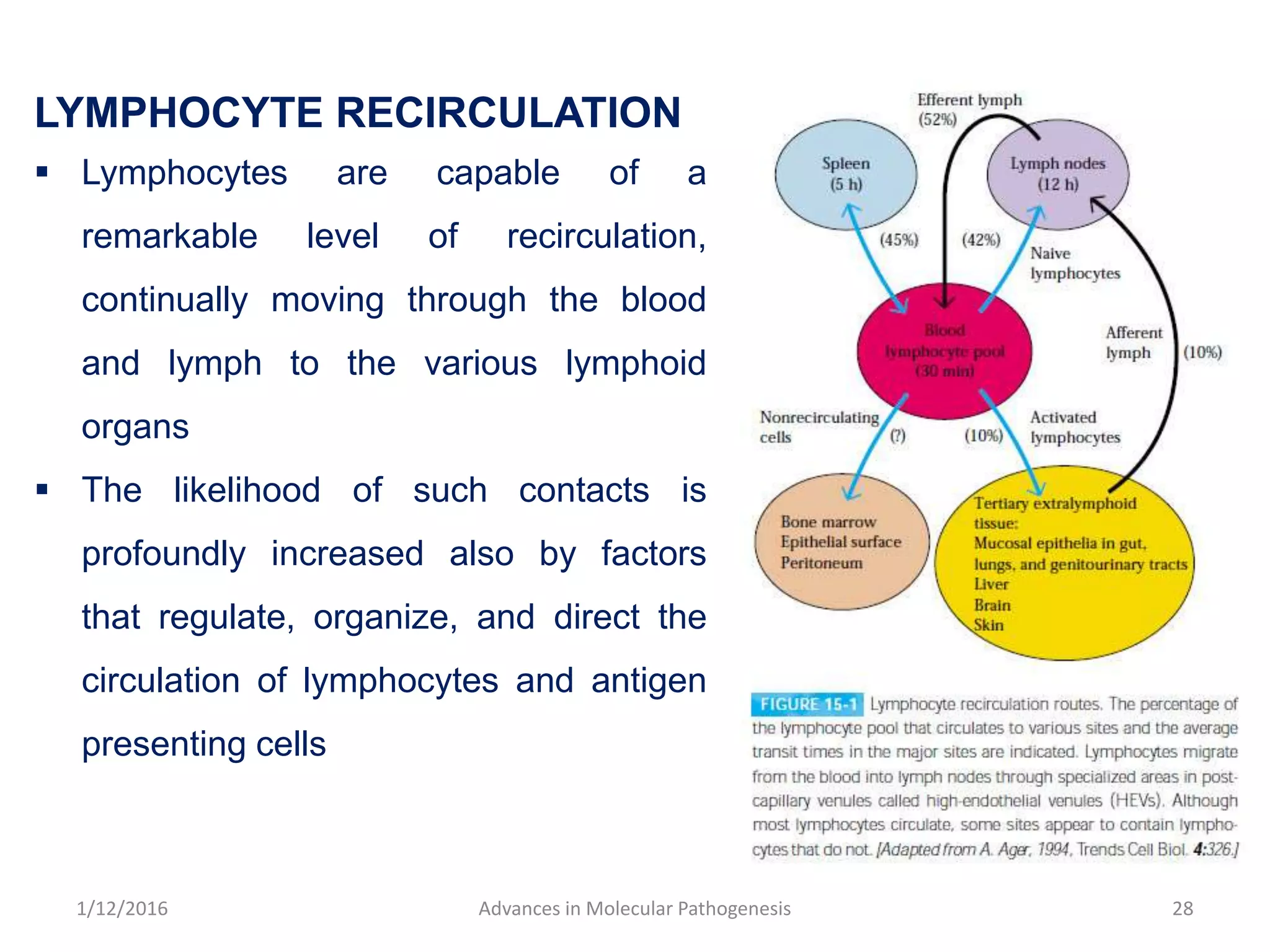
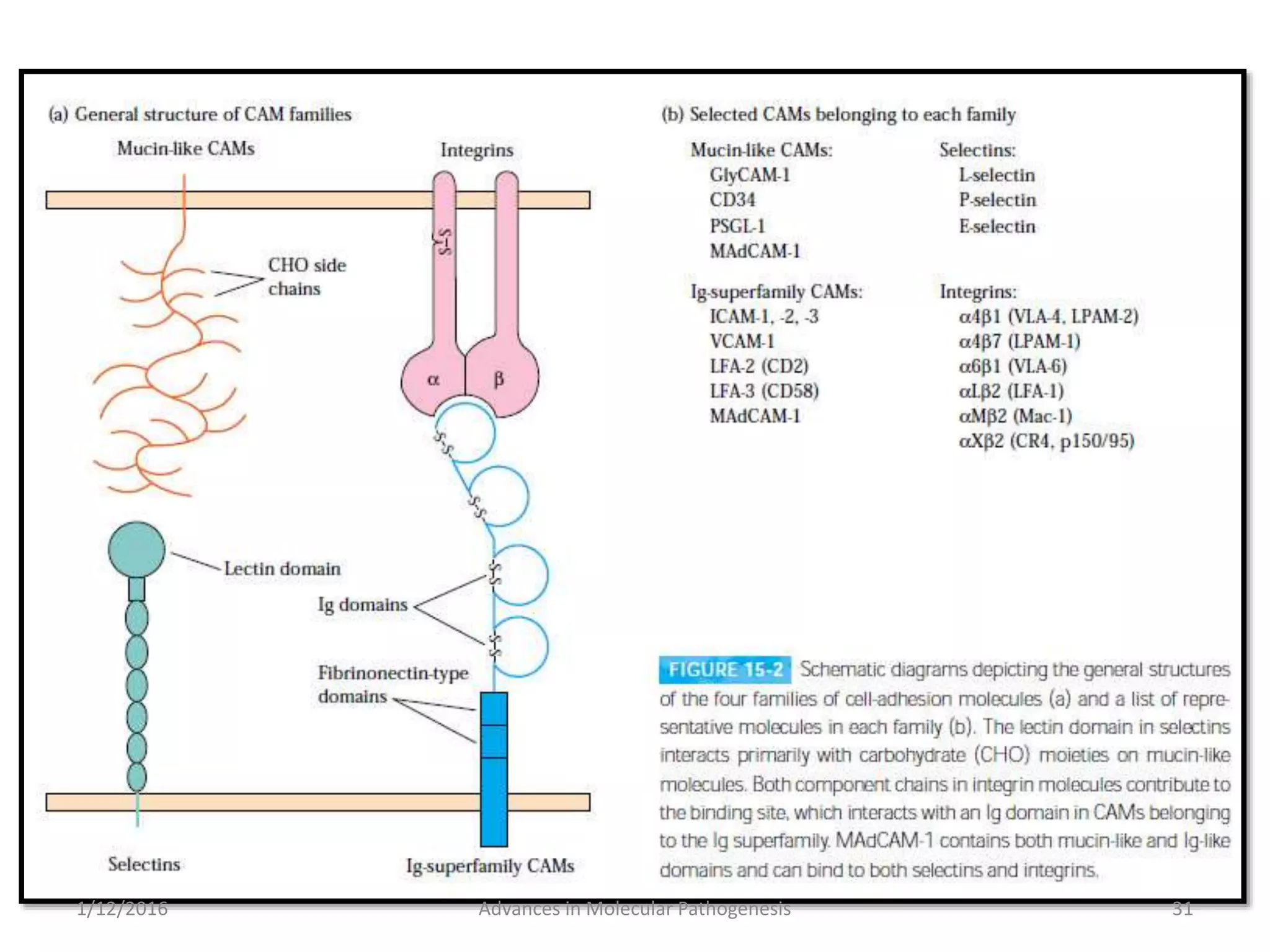
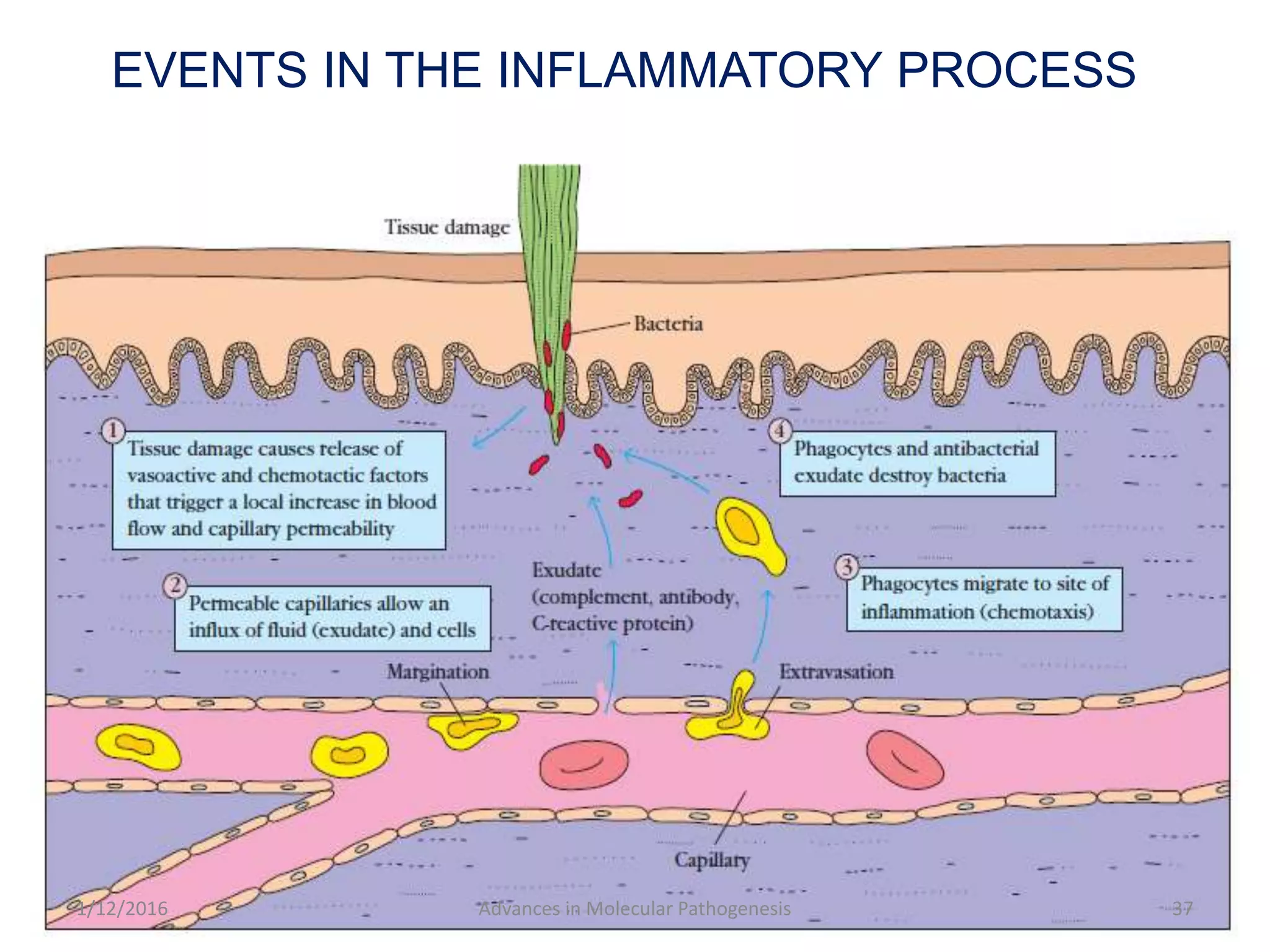
The document discusses the immune system and its innate and adaptive components. It covers the physical, chemical, and cellular barriers that comprise the innate immune system, including barriers in the skin, mucous membranes, and various organ systems. It also describes the complement system and how it functions in immune responses through lysis of cells, opsonization, and inflammation. Adaptive immunity is highlighted as the antigen-specific branch that involves lymphocytes and memory responses.