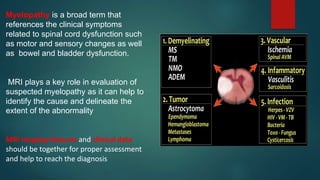
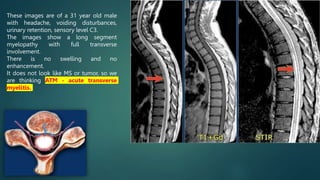
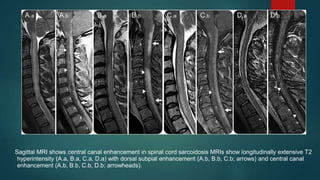
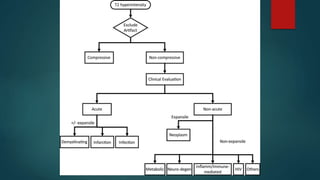
1. MRI plays a key role in evaluating suspected myelopathy by identifying the cause and extent of spinal cord abnormalities.
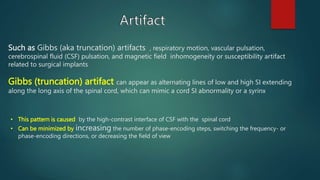
2. Common artifacts that can mimic cord abnormalities include Gibbs artifacts and pulsation artifacts. Extrinsic compression is also considered.
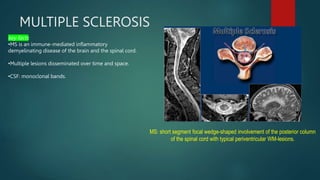
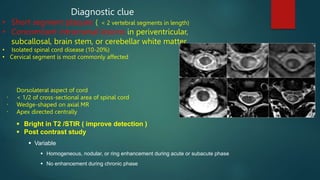
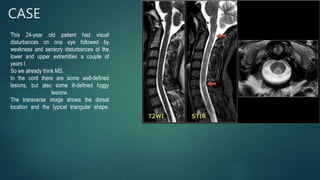
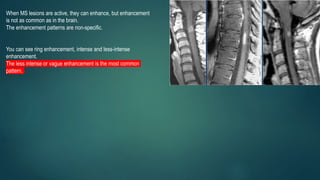
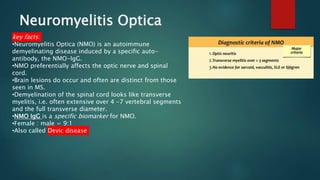
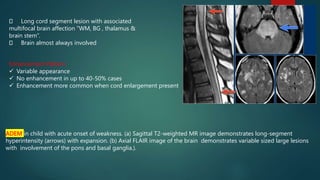
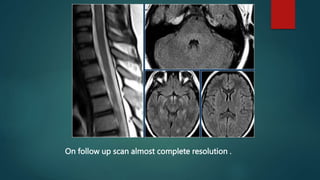
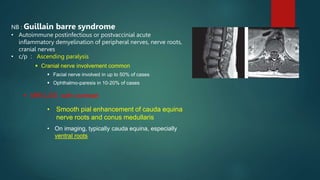
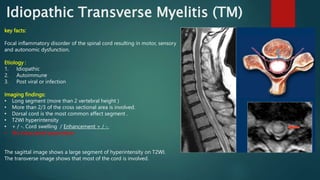
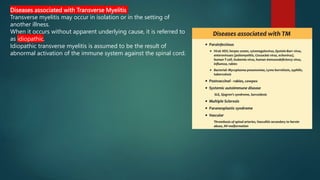
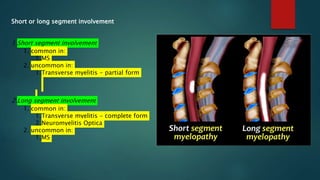
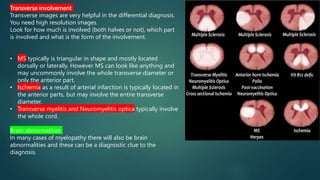
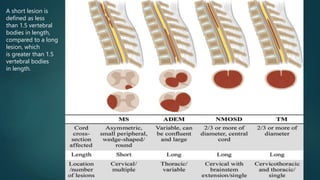
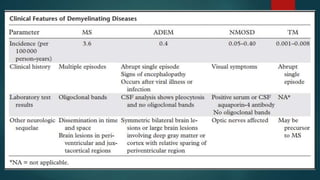
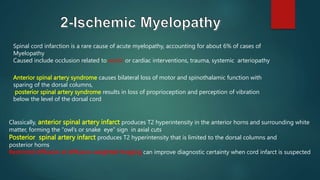
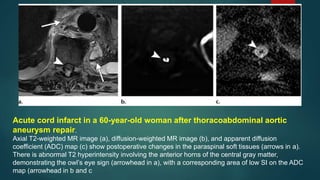
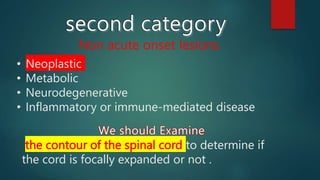
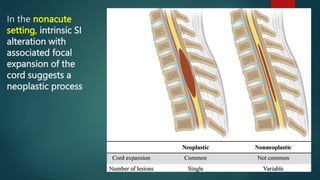
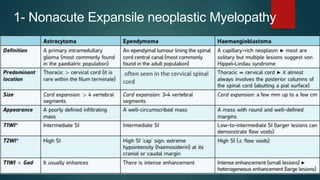
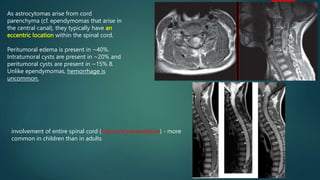
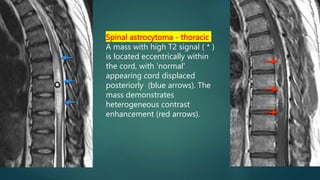
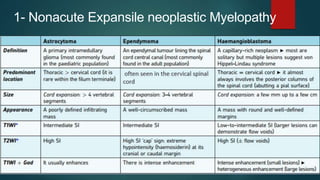
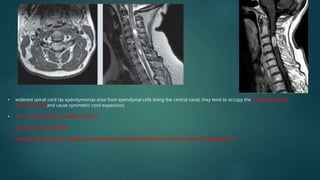
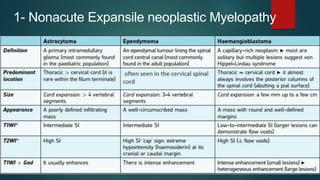
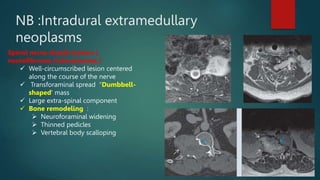
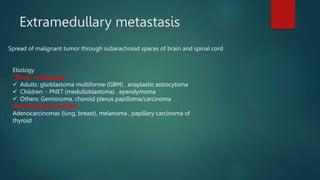
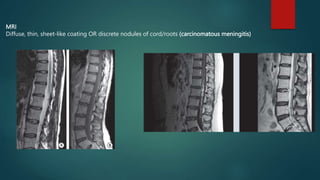
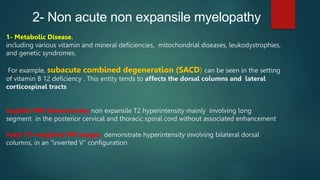
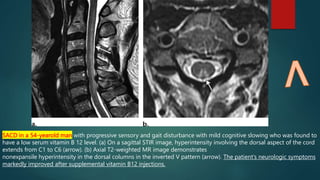
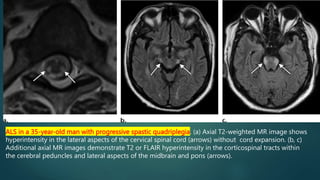
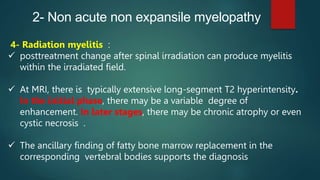
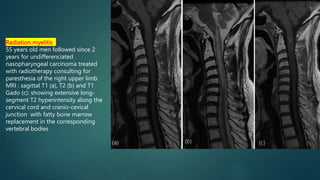
3. For intrinsic cord lesions, the differential depends on acute vs nonacute onset. Acute causes include demyelination, ischemia, infection while nonacute includes neoplasm, metabolic, neurodegenerative, and inflammatory diseases.