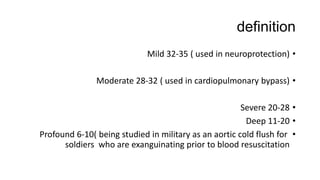
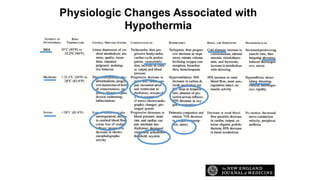
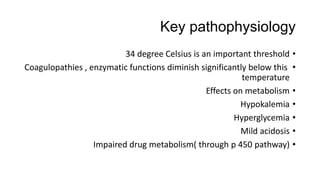
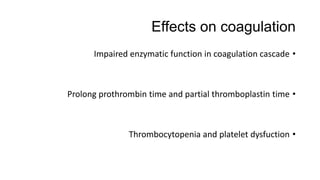
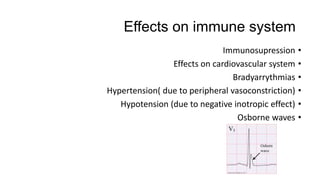
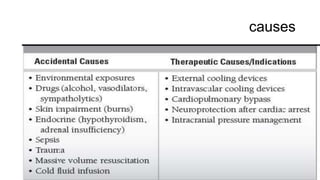
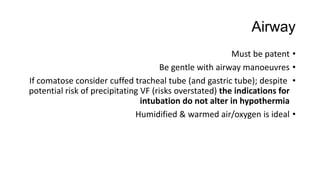
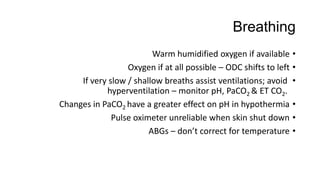
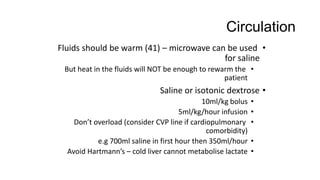
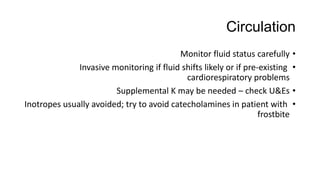
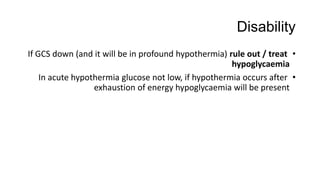
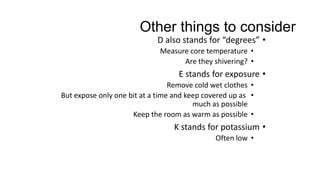
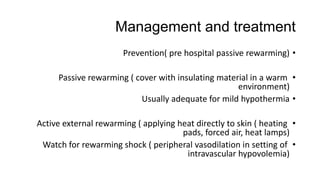
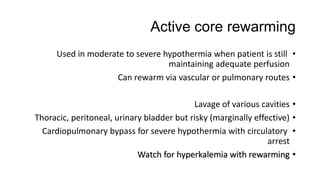
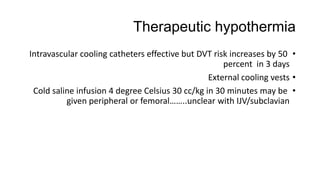
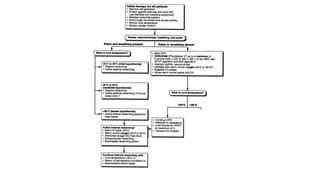
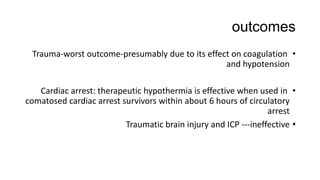
Hypothermia is common in trauma patients and those exposed to cold environments. It can be accidental, primary, secondary, or therapeutic. Mild hypothermia between 32-35 degrees Celsius is used for neuroprotection, while moderate (28-32 degrees) is used for cardiopulmonary bypass. Physiologic changes associated with hypothermia include coagulopathies, metabolic effects, hypokalemia, hyperglycemia, and effects on the cardiovascular, immune, and coagulation systems. Treatment follows the ABCDE approach - ensuring a patent airway, warming humidified oxygen, warm IV fluids, monitoring for hypoglycemia, and passive or active external rewarming depending on severity. Core rewarm