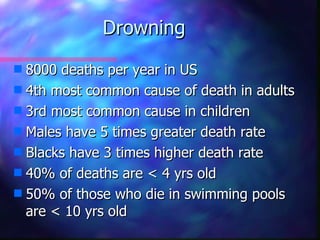
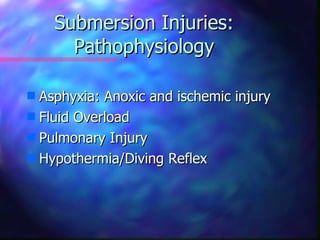
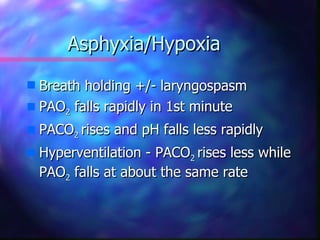
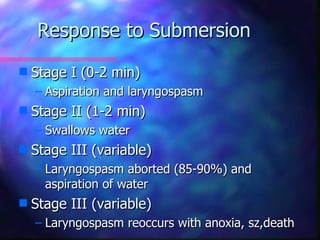
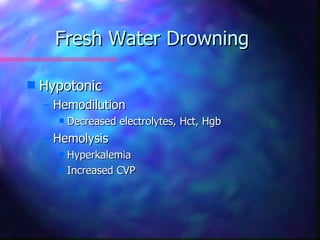
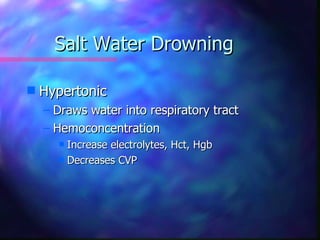
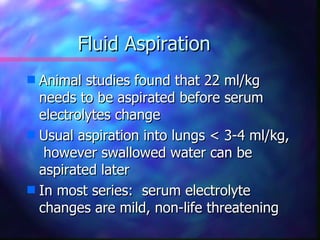
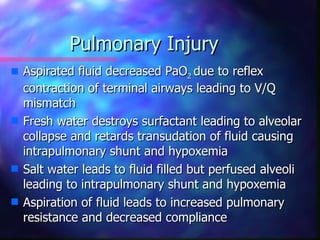
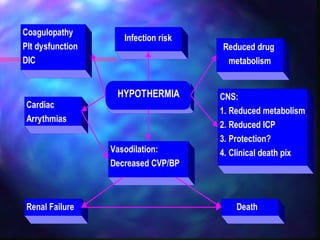
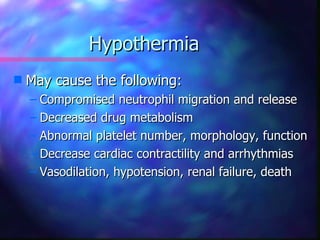
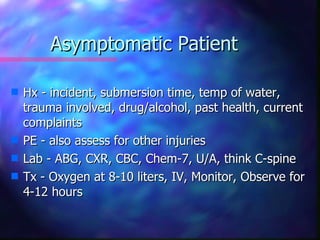
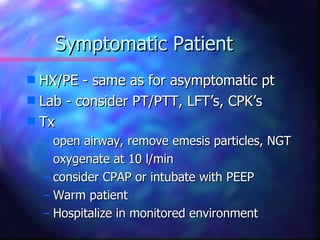
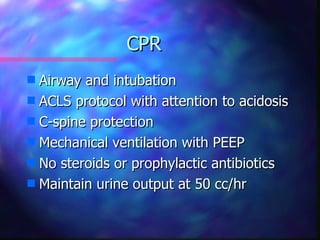
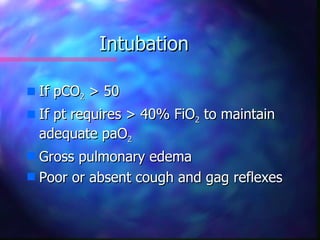
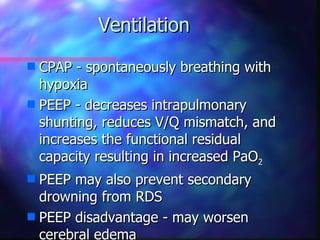
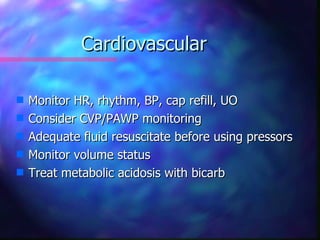
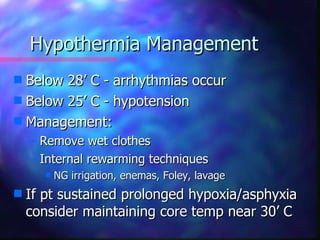
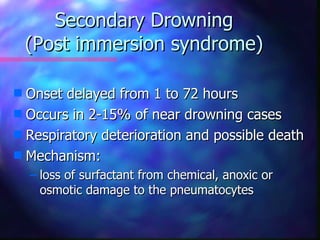
Submersion injuries can cause drowning, near-drowning, or secondary drowning. Drowning is a leading cause of accidental death, especially in children under 5. Near-drowning can cause hypoxic injury, fluid overload, pulmonary injury, and hypothermia. Treatment involves airway management, oxygenation, ventilation, warming, and monitoring for secondary complications. Prognosis depends on factors like submersion time, response to resuscitation, and neurological status. Prevention focuses on education, supervision, and safety measures.