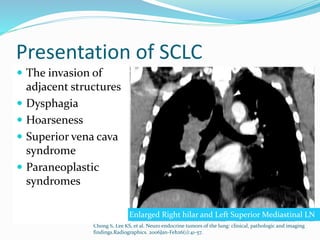
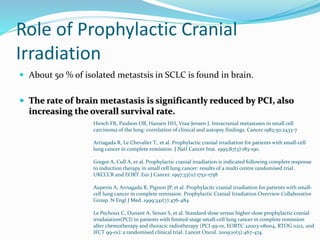
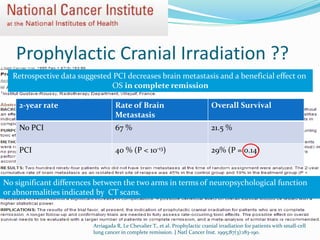
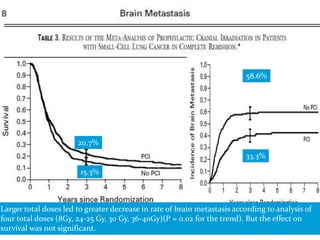
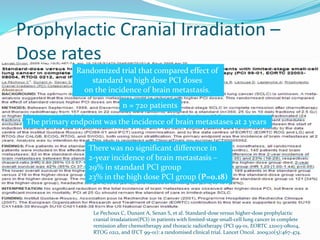
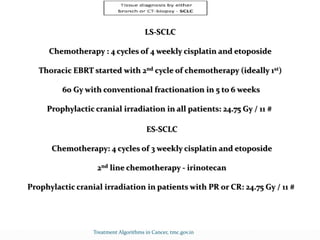
This document summarizes information about small cell lung cancer (SCLC), including its incidence, risk factors, staging, prognosis, diagnostic workup, and treatment approaches. Some key points:
- SCLC accounts for 15-20% of lung cancer cases and has a median age of diagnosis of 64. Most patients are smokers.
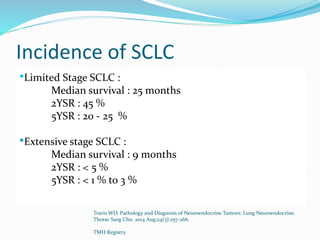
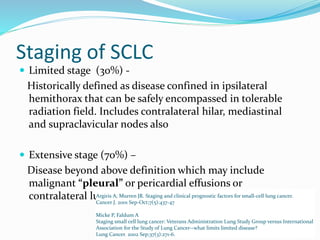
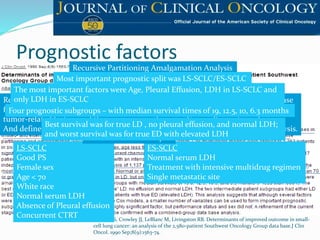
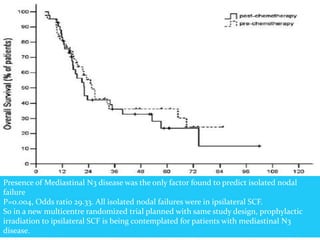
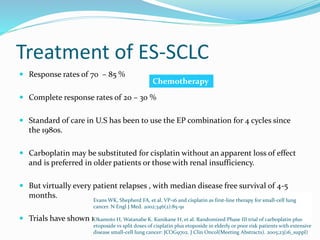
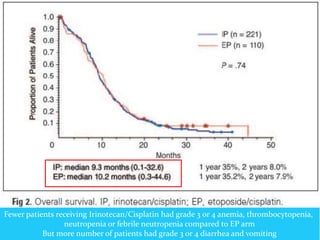
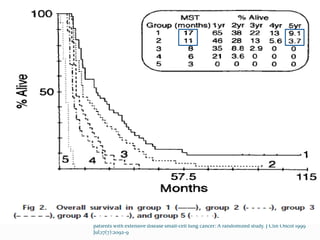
- Limited stage SCLC is confined to one lung and nearby lymph nodes, while extensive stage has spread further. Median survival is 25 months for limited vs 9 months for extensive disease.
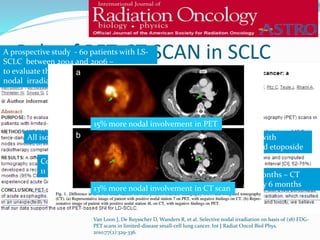
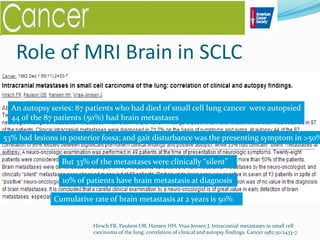
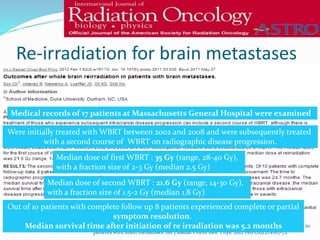
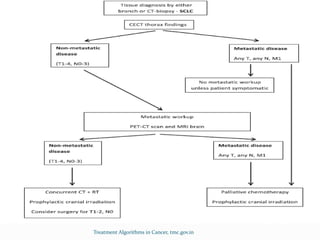
- Workup includes imaging, biopsy, and brain MRI due to the risk of brain metastases. PET-CT helps determine extent of disease.
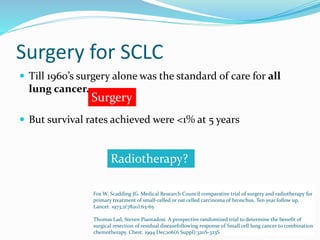
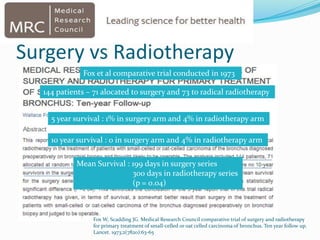
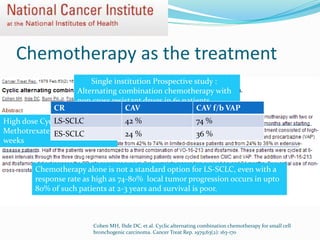
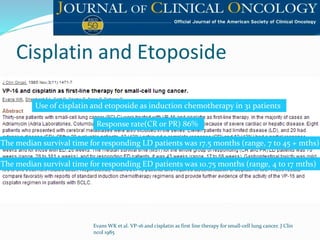
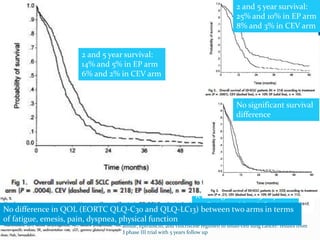
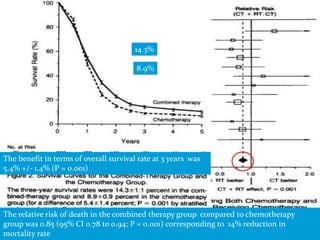
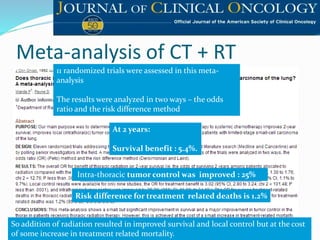
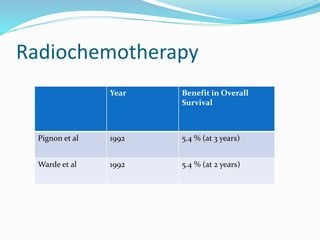
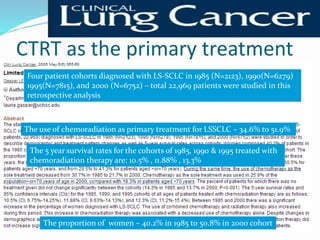
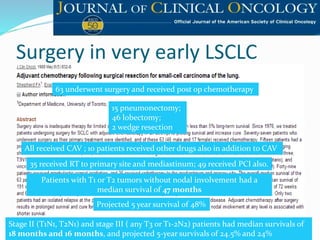
- Historically, surgery and chemotherapy alone did