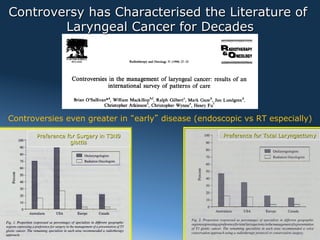
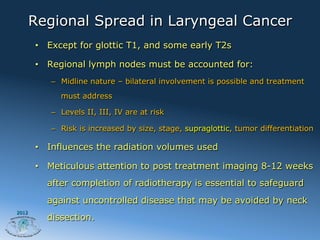
This document discusses radiation therapy for laryngeal cancer preservation. It notes controversies in treatment approaches for early disease. While radiation therapy is a staple in organ preservation strategies, surgical preference remains for T3N0 glottic cancers. The document summarizes treatment approaches and outcomes for different T stages of laryngeal cancer based on studies. It also discusses dose fractionation schedules, advantages of intensity-modulated radiation therapy (IMRT), and technical issues in treating advanced laryngeal cancer with radiation therapy.















![Dose Fractionation in Early Disease
• Yu et al., 1997 [1]
– Retrospective study – 5 yr local ctr rate of XRT on T1
glottic CA
– Daily fx > 2 Gy (50 Gy/2.5Gy QD & 65.25Gy/2.25 Gy QD)
had 5 yr local ctr rate of 84%
– Daily fx = 2 Gy had 5 yr local ctr 65.6%
• Yamazaki et al., 2006 [2]
– RTC – in T1 glottic CA addressing dose per fraction
• Andy Trotti et al, RTOG 95-12 – closed [3]
– Randomized pts with T2 glottic cancer to 70Gy/2Gy QD vs
79.2 Gy/1.2 Gy BID
2012
1 Yu E. et al., Int J Radiat Oncol Biol Phys. 1997 Feb 1;37(3):587-91
2 Yamazaki H et al., Int J Radiat Oncol Biol Phys. 2006 Jan 1;64(1):77-82
3 Trotti A, IJRBOP Volume 66, Issue 3, Supplement 1, 1 November 2006, Page S15](https://image.slidesharecdn.com/mradiationtherapyforlaryngealfunctionpreservation-os-121009062704-phpapp01/85/Radiation-therapy-for-laryngeal-function-preservation-by-Brian-O-Sullivan-19-320.jpg)



















