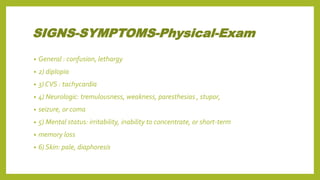
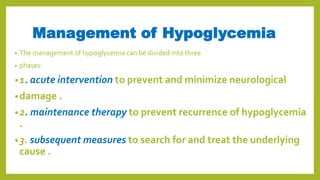
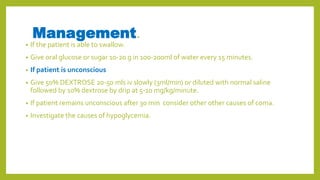
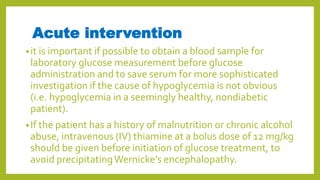
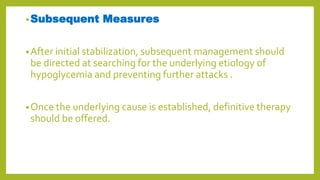
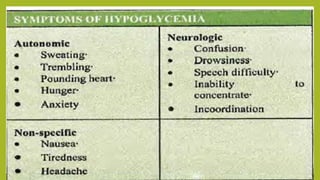
Hypoglycemia, or low blood sugar, is caused by very low levels of blood glucose, below 3.0 mmol/L. It is common in type 1 diabetes and can occur due to overdose of insulin or diabetes medications, excessive alcohol consumption, or certain illnesses. Symptoms range from irregular heartbeat and sweating to confusion and loss of consciousness. Treatment involves giving the person glucose tablets, juice, or an IV glucose solution to quickly raise their blood sugar levels. Preventing hypoglycemia requires education on recognizing symptoms early and always having access to fast-acting carbohydrates.
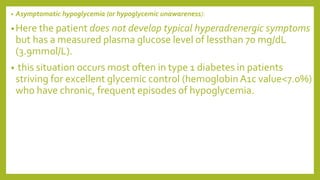
![•Relative hypoglycemia: in which a patient experiences hyperadrenergic
hypoglycemic symptoms but has a measured plasma glucose level greater than 70 mg/dL (3.9
mmol/L).
• this situation occurs most often in patients who have had months (or
• longer) of hyperglycemia (plasma glucose levels >200 mg/dL[11.1mmol/L] at all times) whose
plasma glucose levels are then lowered by medication or lifestyle changes closer to the
normalrange.
• Hyperadrenergic hypoglycemic symptoms can occur when the
• plasma glucose level in these patients is 120 mg/dL (6.7 mmol/L) or
• even higher.
• If these patients continue to keep their plasma glucose level substantially less than 200 mg/dL
(11.1 mmol/L), the threshold at which they manifest hypoglycemic symptoms will fall to more
typicallevels (<70 mg/dL [3.9mmol/L]).](https://image.slidesharecdn.com/hypoglycemia-200302145521/85/Hypoglycemia-19-320.jpg)