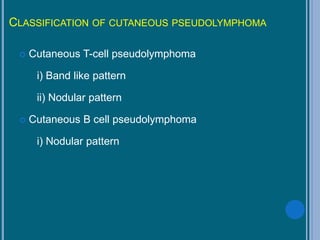
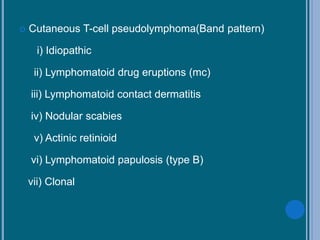
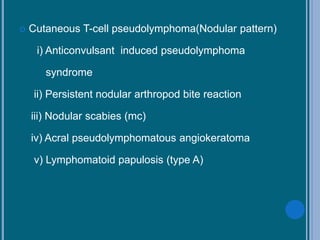
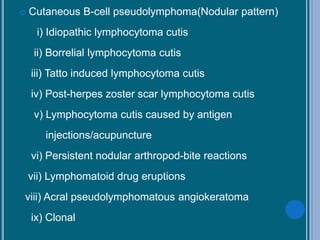
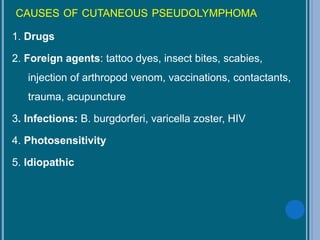
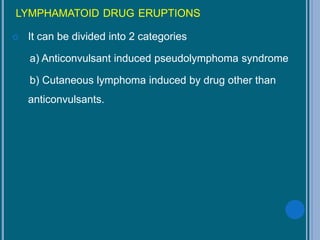
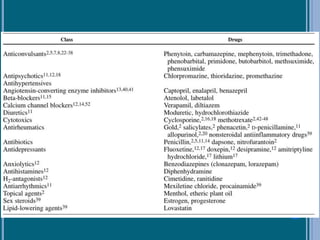
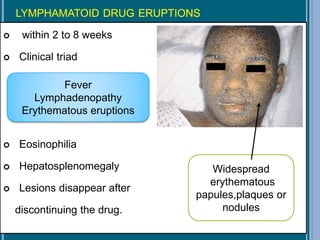
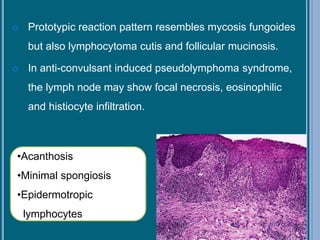
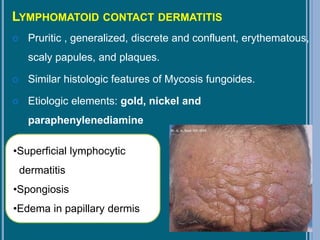
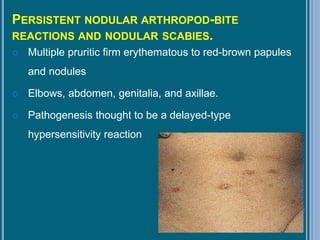
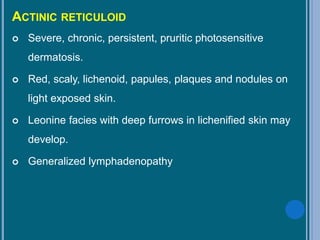
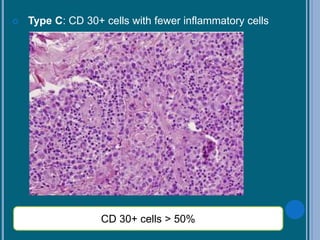
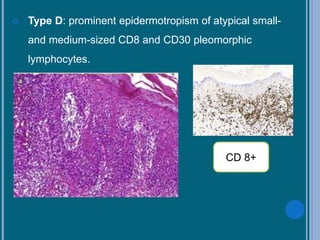
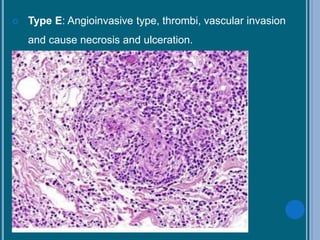
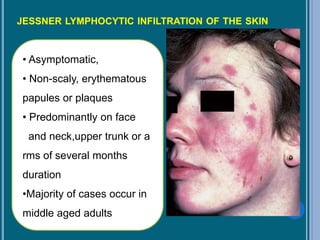
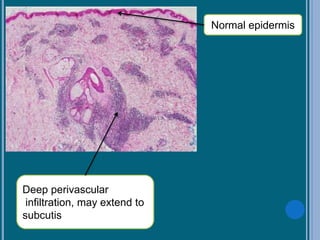
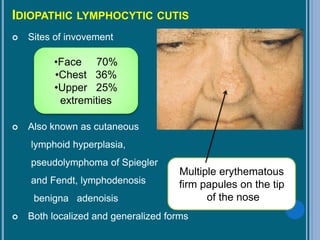
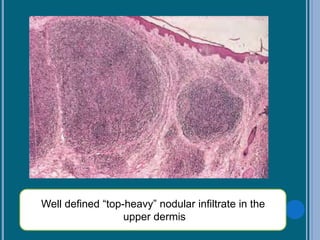
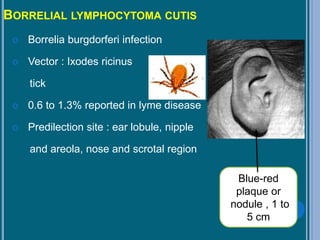
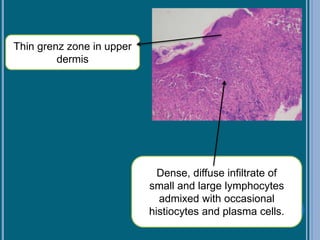
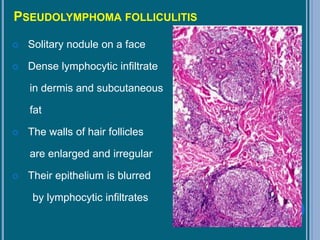
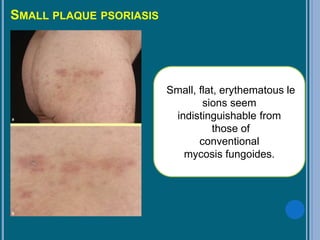
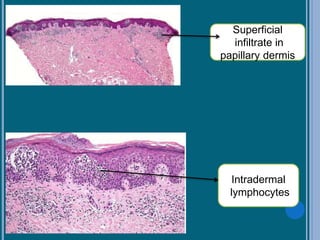
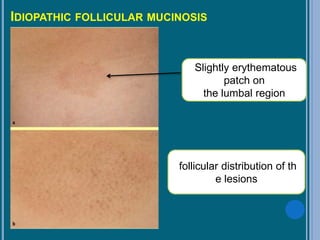
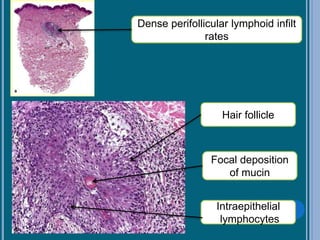
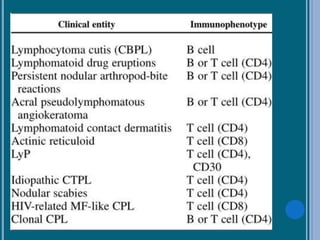
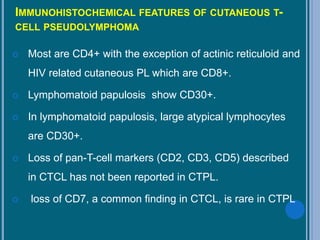
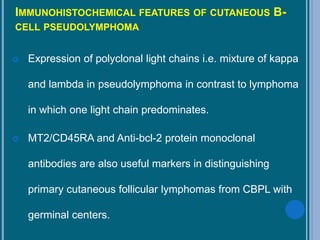
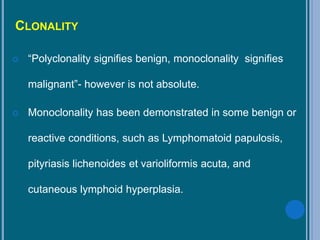
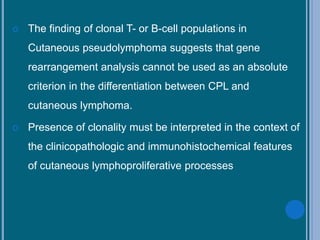
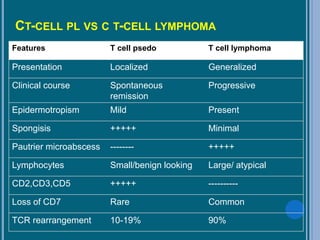
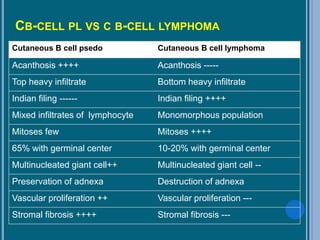
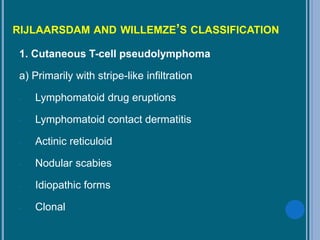
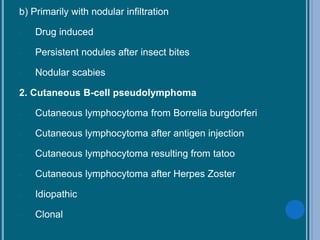
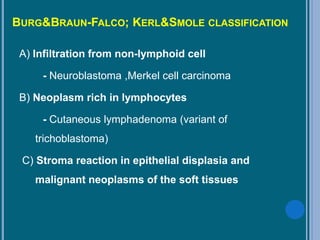
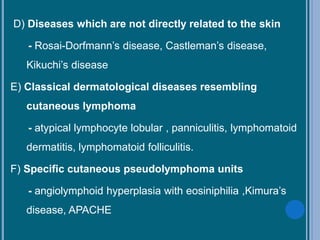
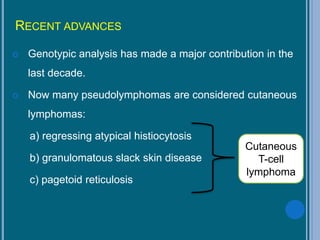
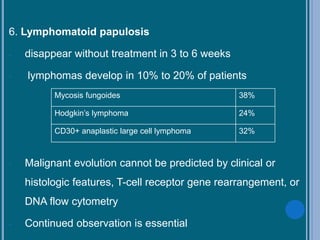
Cutaneous pseudolymphoma (CPL) is a benign process that simulates lymphoma and can present in various forms, classified into cutaneous T-cell and B-cell pseudolymphomas based on histological patterns. The document discusses historical aspects, definitions, etiological factors, clinical features, and the pathogenesis of CPL, including specific drug-related eruptions and infections as causes. Management strategies vary based on the type of pseudolymphoma, with many cases resolving after discontinuing the inciting agent or requiring other treatments.