This document provides information about hysterosalpingography (HSG) and fistulogram procedures. It describes:
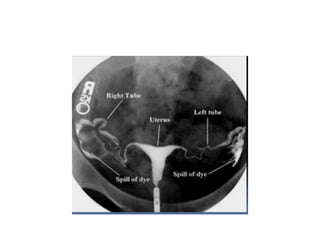
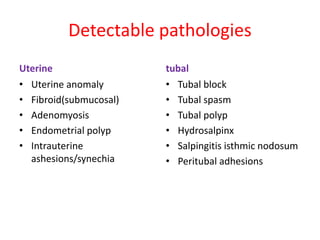
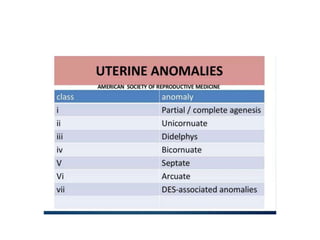
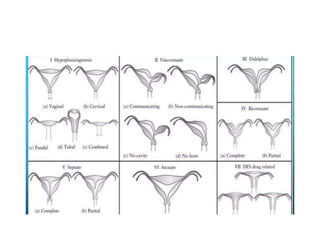
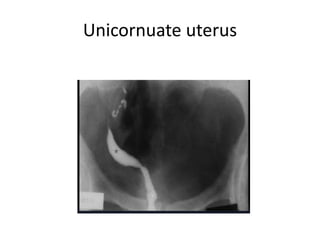
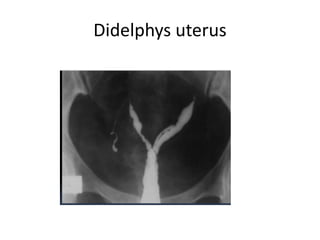
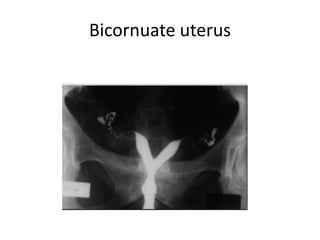
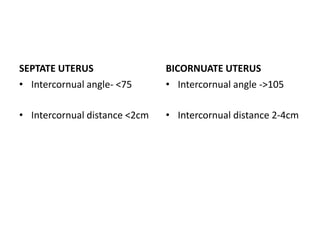
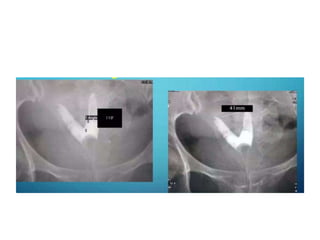
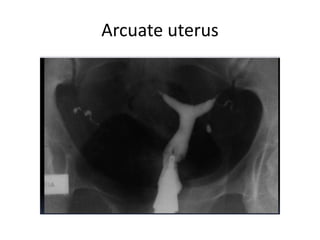
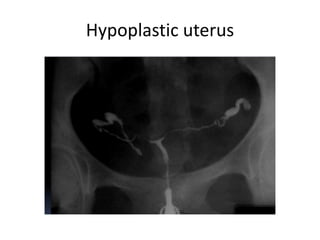
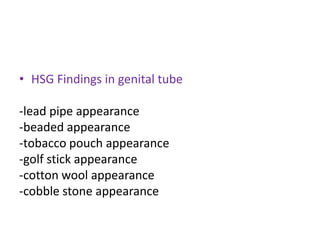
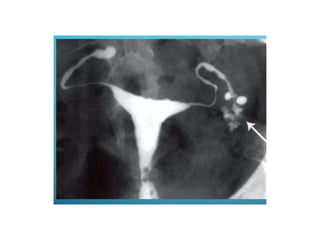
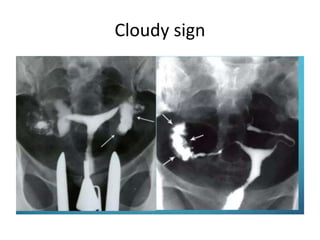
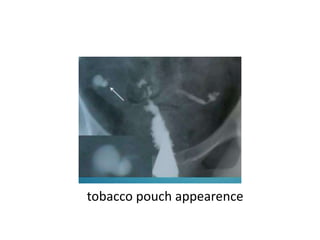
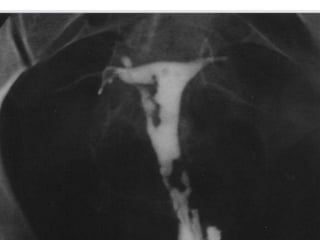
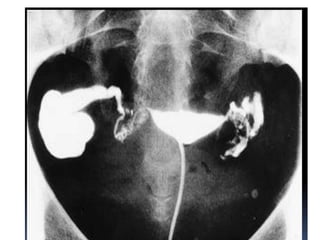
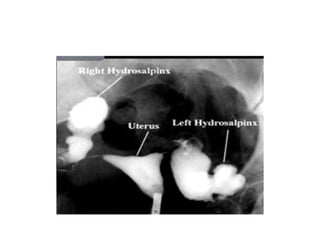
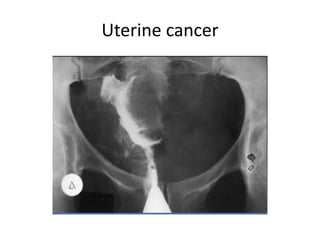
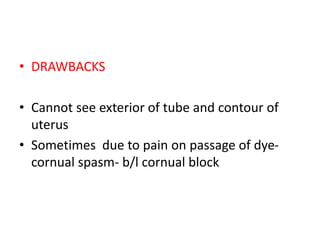
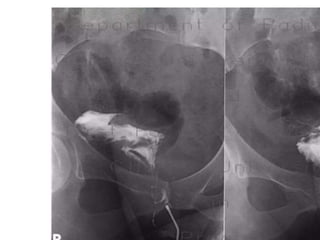
- HSG is used to evaluate the uterine cavity and fallopian tubes by injecting radio-opaque dye through the cervix. It can detect abnormalities in the shape of the uterus and fallopian tube blockages.
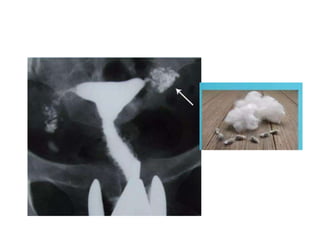
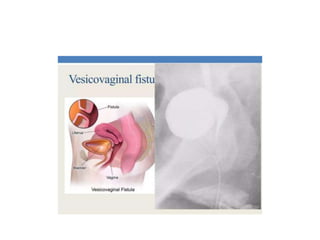
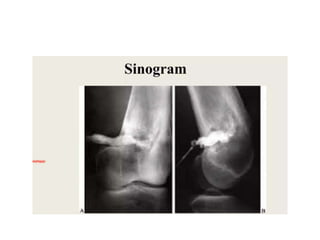
- A fistulogram uses injected contrast dye to visualize and determine the route and extent of abnormal passages like fistulas or sinuses.
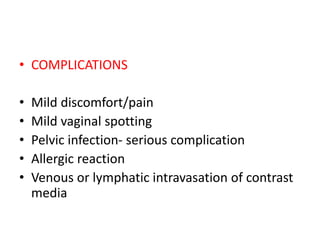
- Both procedures require informed consent and have risks like discomfort, infection or allergic reaction to the contrast dye. Precautions are taken to perform them aseptically and accurately map any abnormalities found.