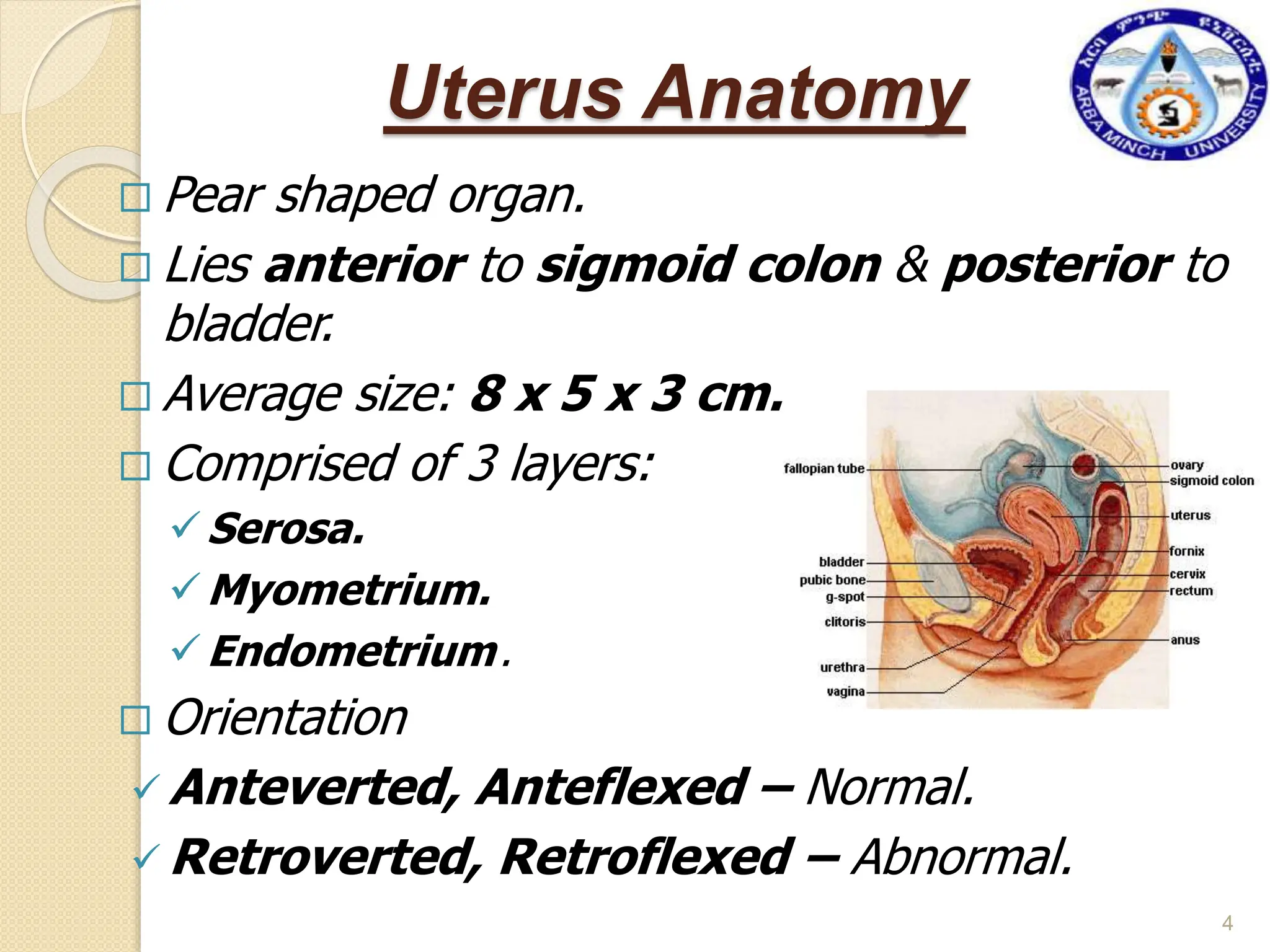
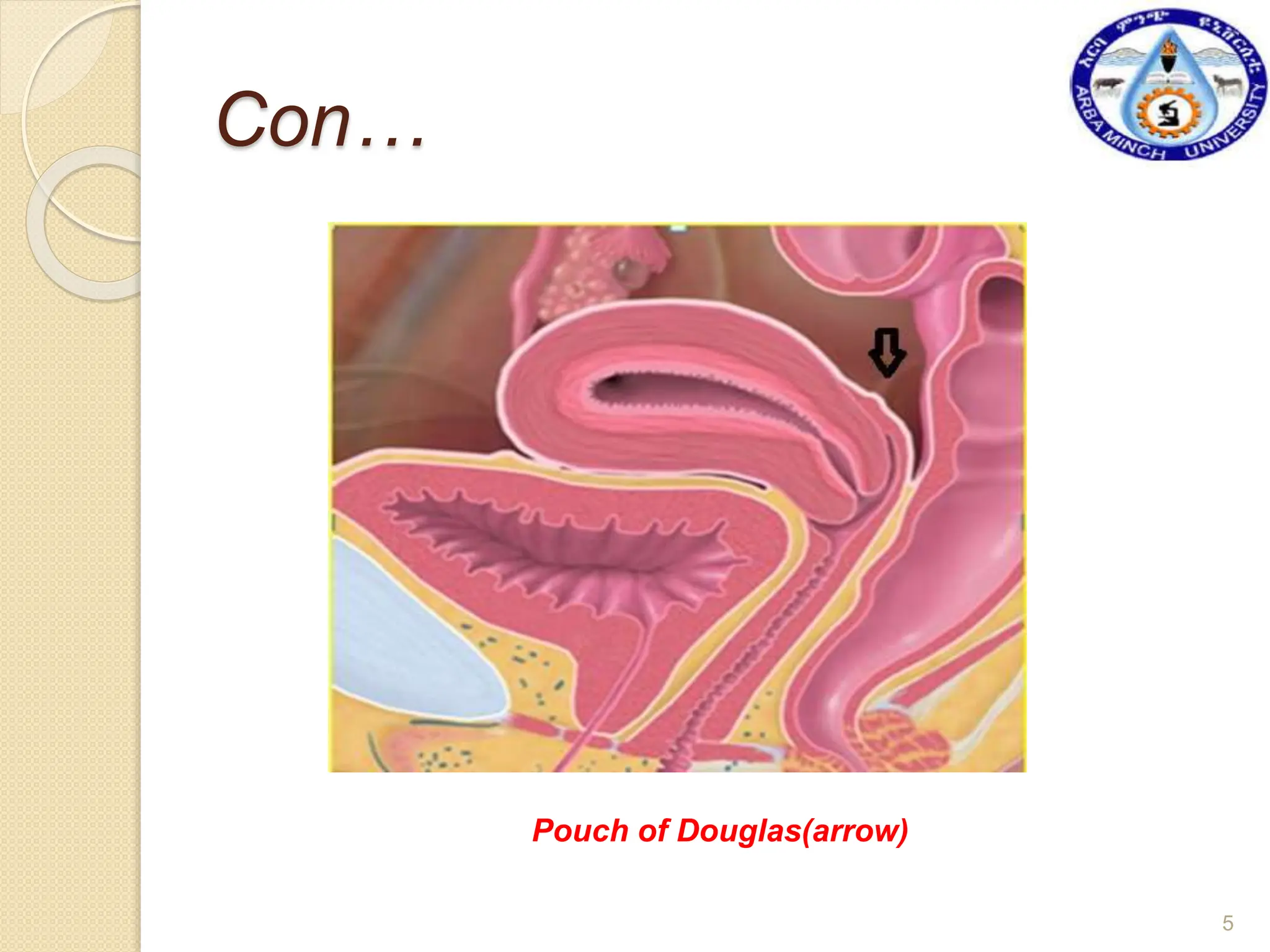
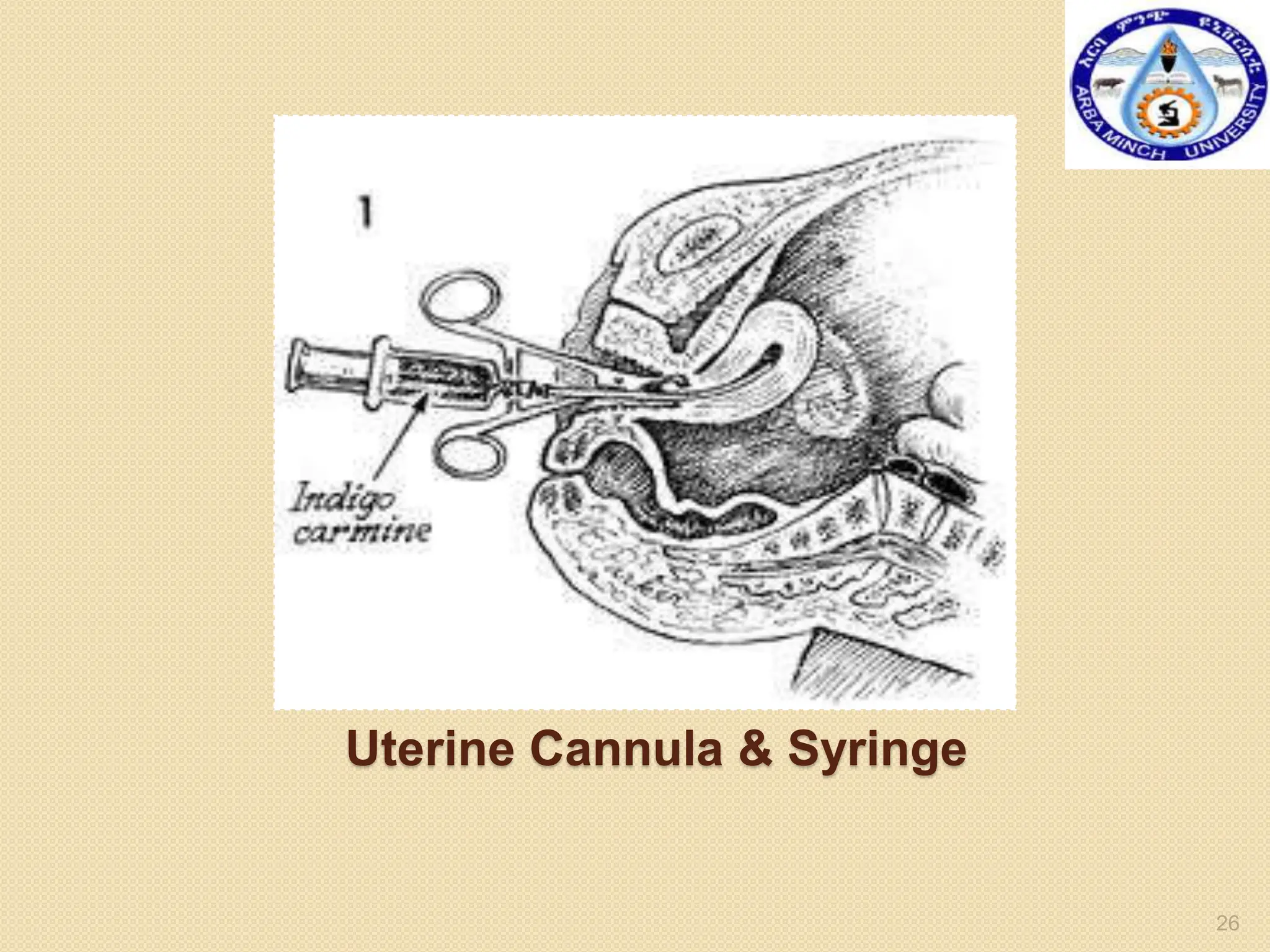
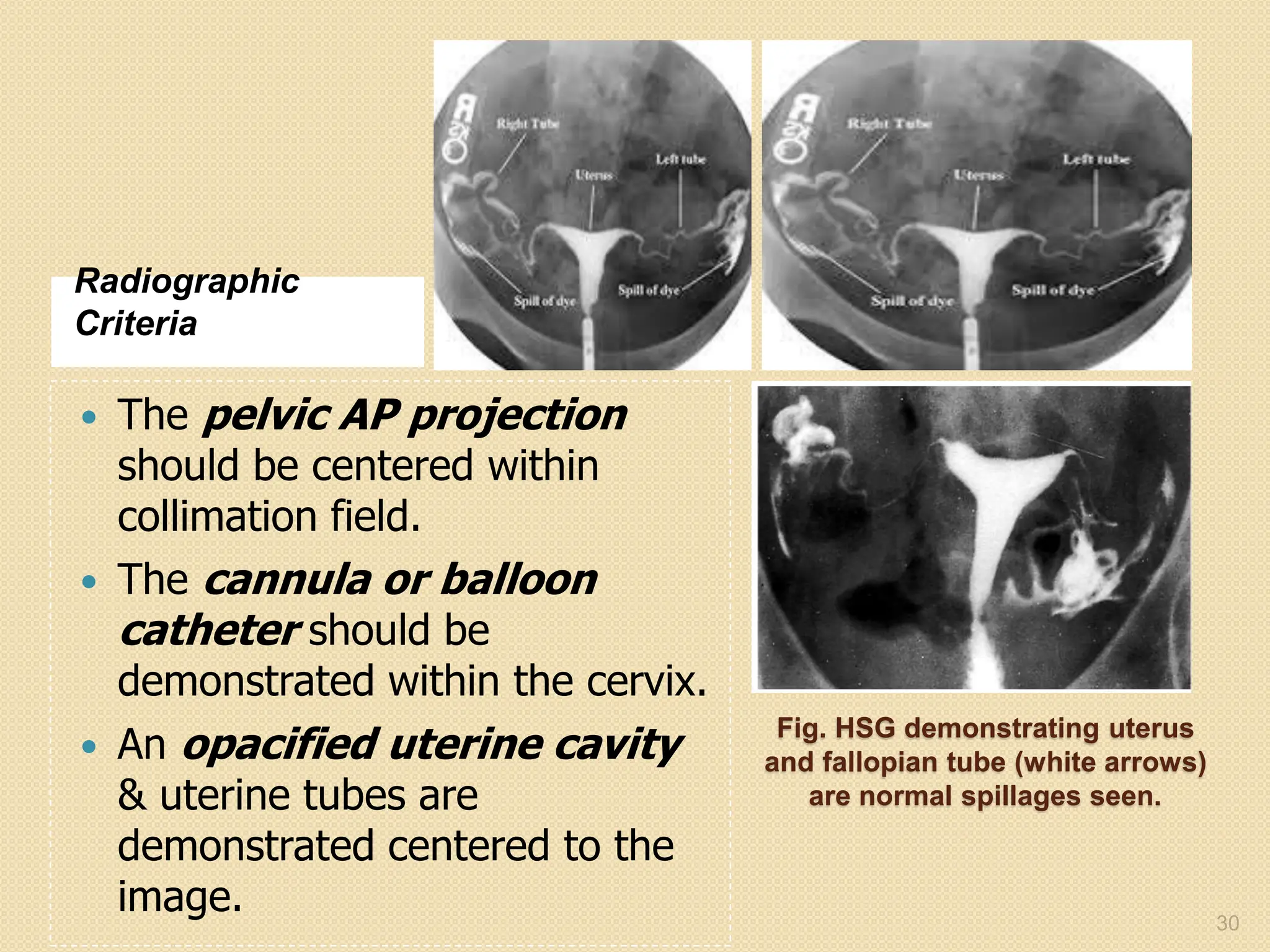
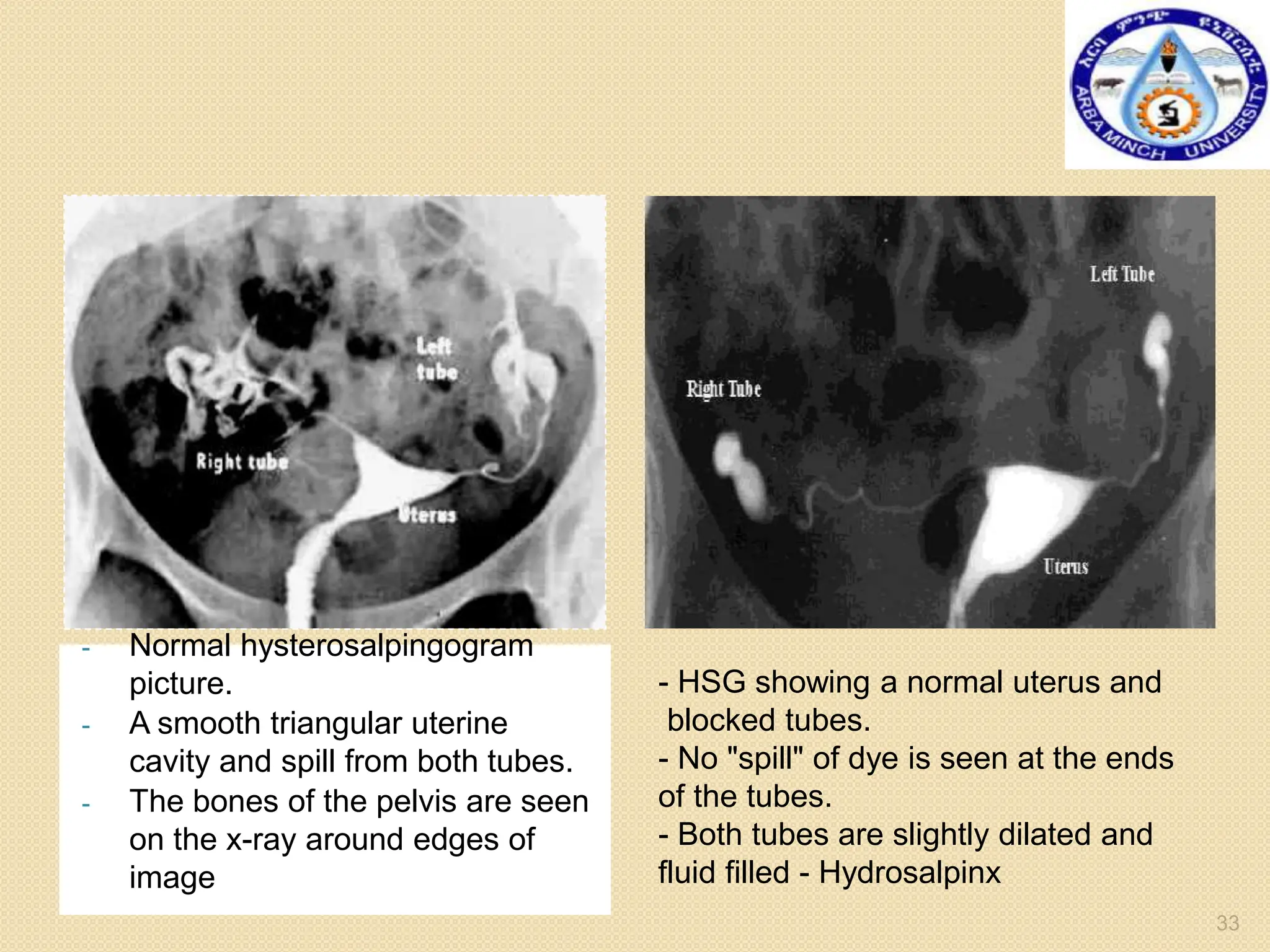
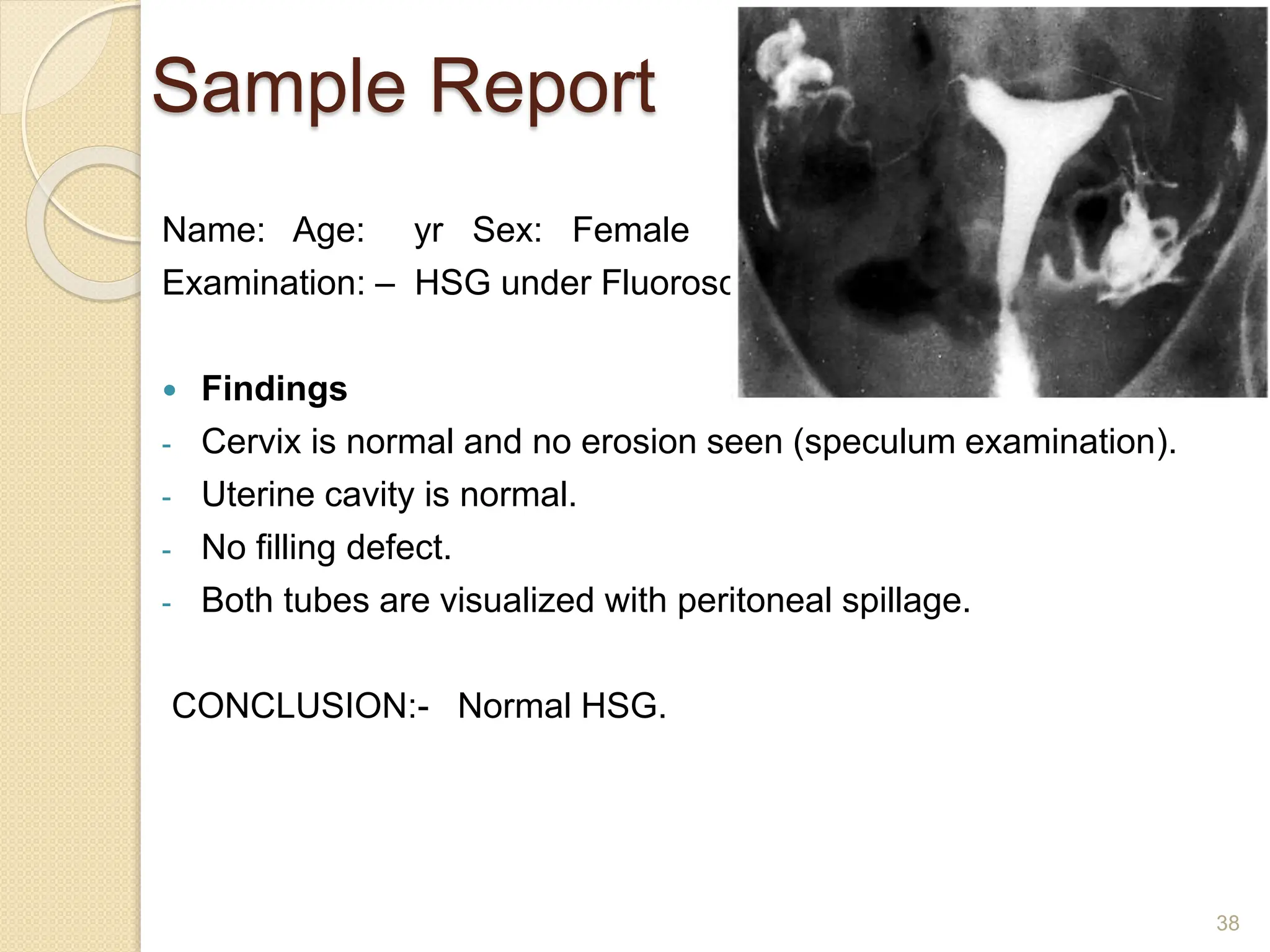
This document provides information about hysterosalpingography (HSG), a radiographic examination of the female reproductive tract. It begins by outlining the objectives and describing the anatomy of the female genital tract, including the uterus, fallopian tubes, and surrounding structures. It then discusses HSG indications, contraindications, equipment, procedures, imaging techniques, potential findings, and complications. HSG is used to evaluate infertility and detect uterine or fallopian tube abnormalities by injecting contrast medium and imaging its flow through the reproductive tract. The summary provides an overview of the key points covered in the document.