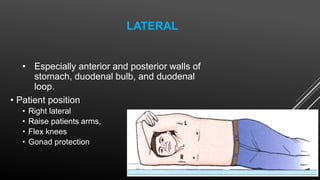
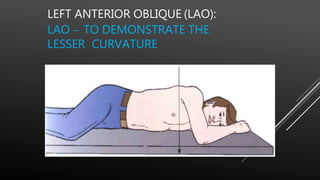
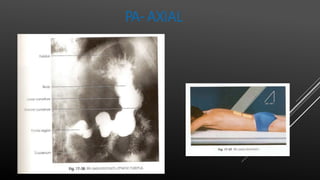
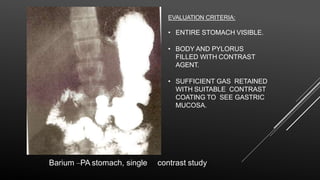
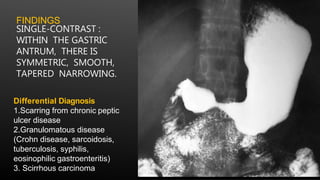
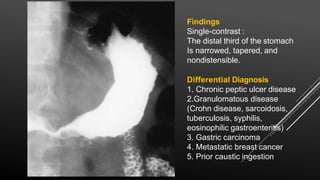
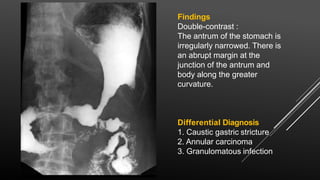
The document provides information about barium meal examinations, including indications, contraindications, preparation, techniques, and findings. It describes single contrast and double contrast barium meal studies. Key points include:
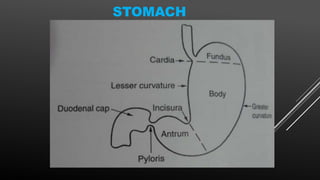
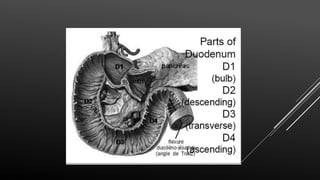
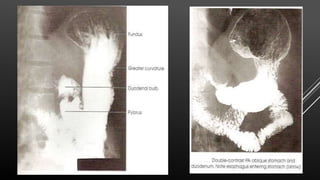
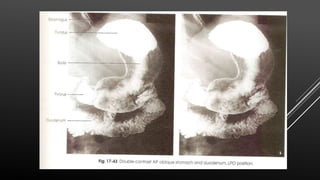
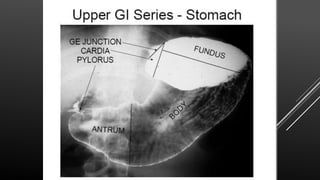
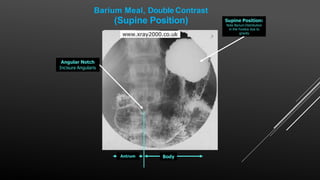
- Barium meal examines the esophagus, stomach, duodenum and proximal jejunum through oral administration of barium contrast.
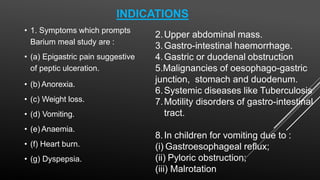
- Indications include abdominal pain, weight loss, vomiting, anemia, and suspected masses or malignancies.
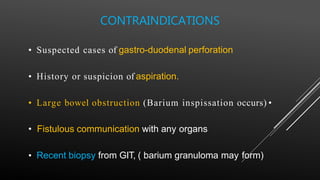
- Contraindications include suspected perforation and recent biopsies.
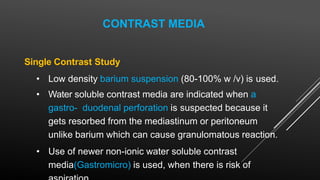
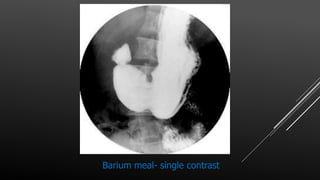
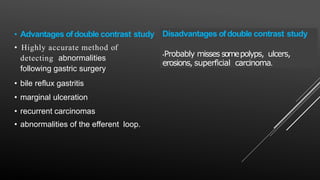
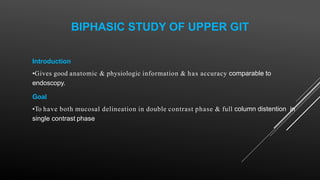
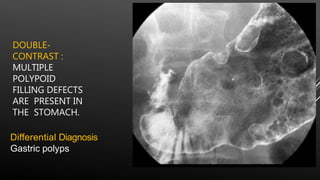
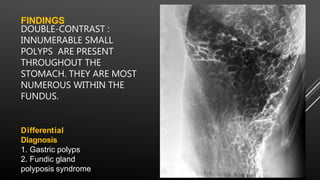
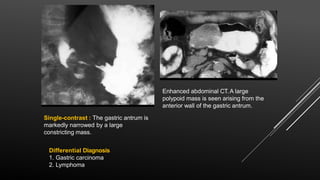
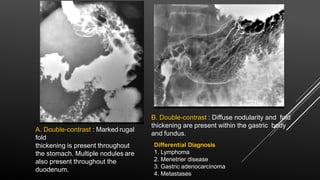
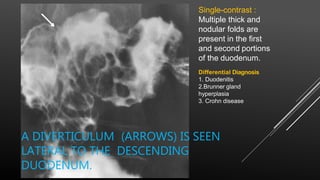
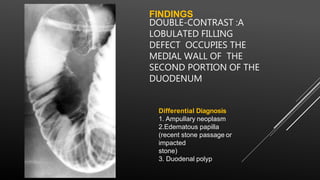
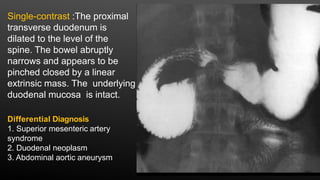
- Single contrast visually assesses anatomy while double contrast enhances mucosal details through added gas contrast.
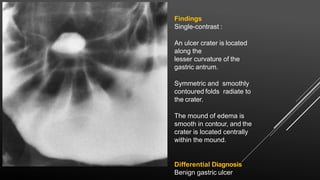
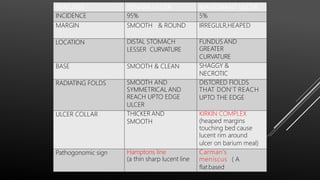
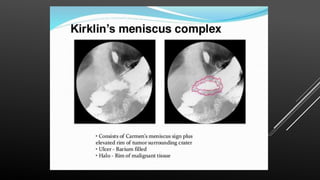
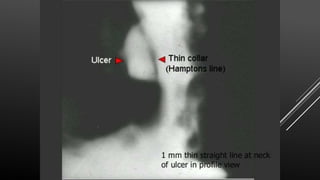
- Findings are evaluated for abnormalities like ulcers,