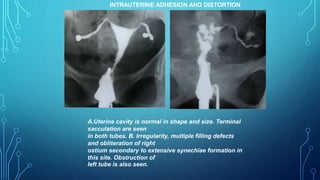
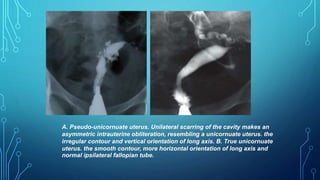
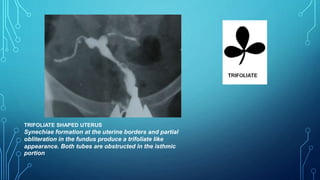
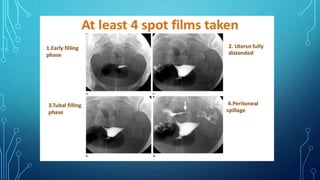
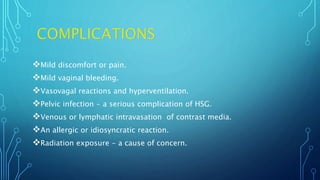
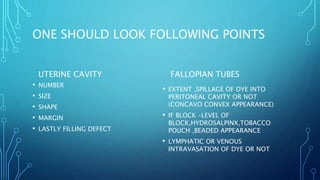
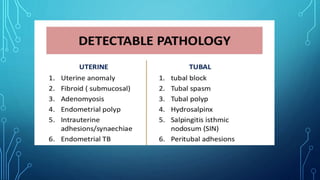
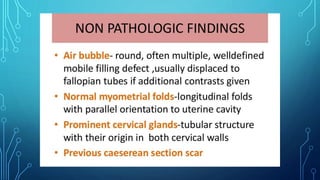
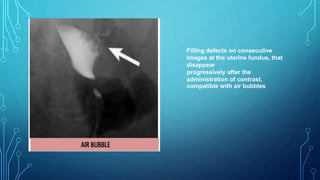
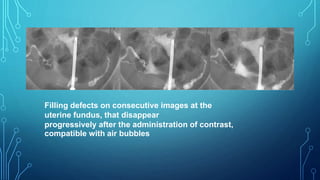
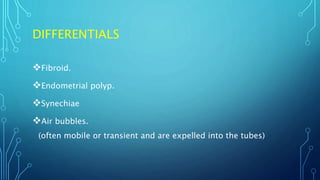
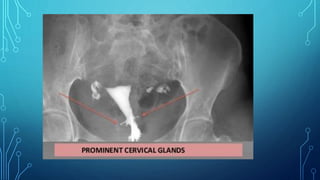
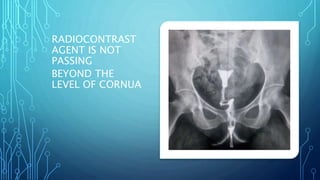
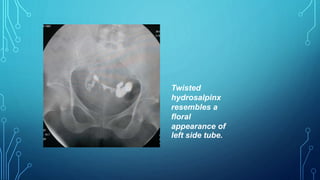
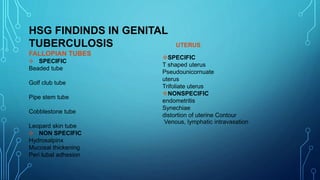
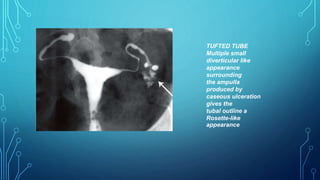
The document describes a hysterosalpingography procedure used to evaluate the uterine cavity and fallopian tubes. Key points include: HSG involves injecting radiopaque contrast medium under fluoroscopy to visualize the uterus and tubes. It is commonly used to investigate infertility. The procedure involves catheterizing the cervix and injecting contrast. Findings are interpreted to evaluate for abnormalities like tubal blockages. Common findings and their differential diagnoses are discussed. Risks are generally minor but can include infection, reaction to contrast, or radiation exposure.







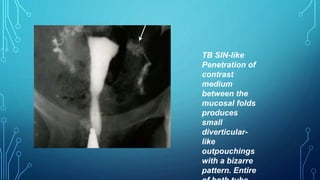
![cotton-wool plug appearance
Distribution of contrast medium in a
reticular pattern
producing a " cotton-wool plug"
appearance [arrow]](https://image.slidesharecdn.com/hsgpptnaba-181003170823/85/Hsg-ppt-38-320.jpg)
![BEADED TUBE
Multiple constrictions along the
fallopian tube giving rise to
a " beaded" appearance [arrows]](https://image.slidesharecdn.com/hsgpptnaba-181003170823/85/Hsg-ppt-39-320.jpg)