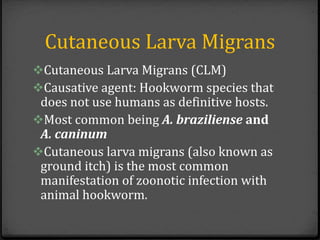
An outbreak of cutaneous larva migrans occurred at a children's summer camp in Miami, Florida in 2006. A total of 22 campers and staff were diagnosed. The outbreak was traced to a sandbox in the playground area that was contaminated with animal feces containing hookworm larvae. Campers who played barefoot in the sandbox were most at risk. Public health officials worked with the camp to remove the contaminated sand and prevent further infections.















![Things considered
• Additional possible sources of exposure considered
included 1) having pets at home (10 patients [45%];
eight dogs, one cat, one unknown); 2) being exposed
to another nearby beach in the week before symptom
onset (nine [41%]); and 3) sharing personal items
such as towels or clothes with other campers (four
[18%]).
• After analyzing initial data collected during July 19--
25, MDCHD suspected that the sandbox
was the source of infection.](https://image.slidesharecdn.com/c142edfc-0ca0-48dd-98b9-837cc5ff2d75-151225020727/85/Hookworm-Larva-Migrans-Presentation-17-320.jpg)

