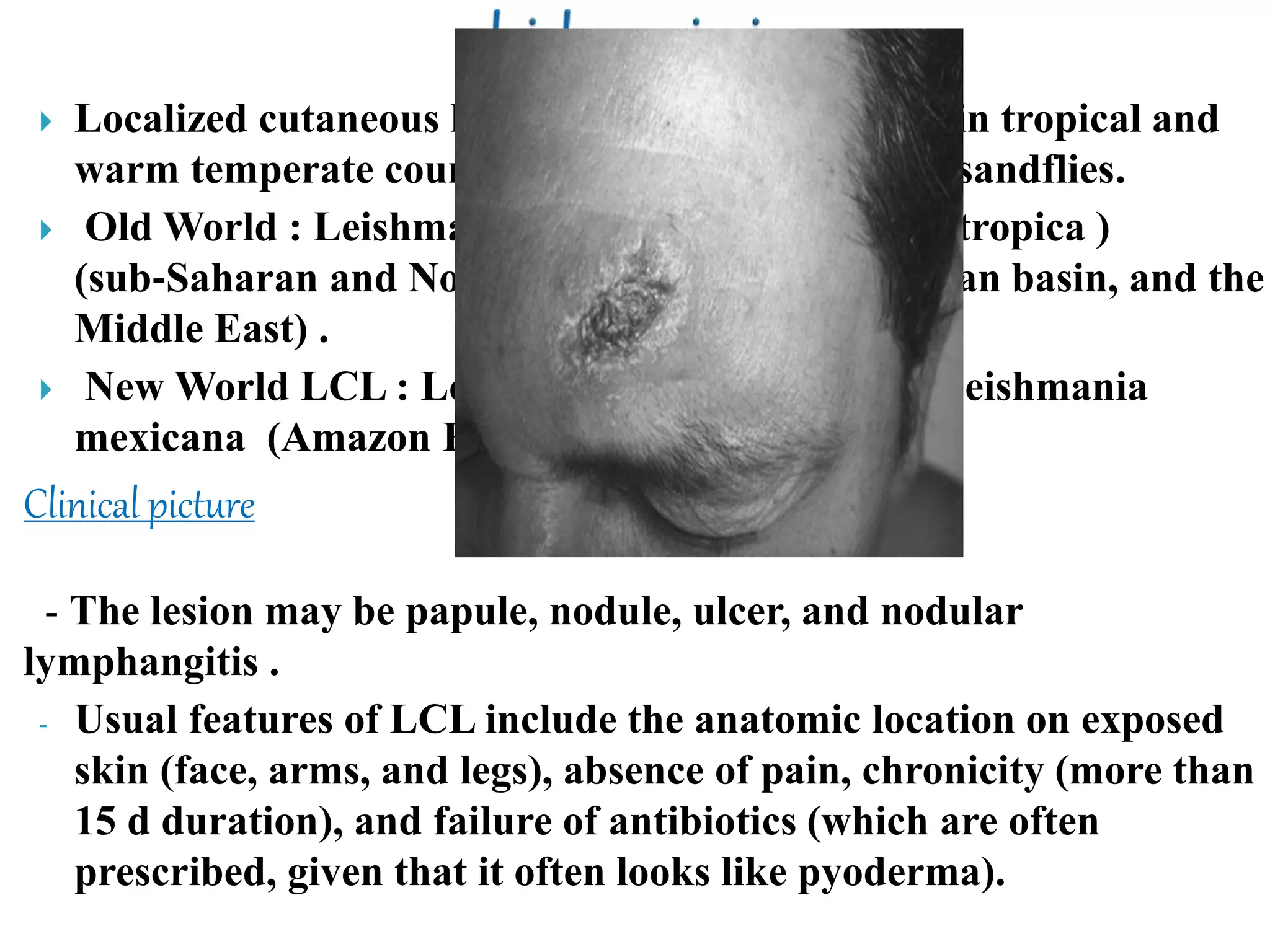
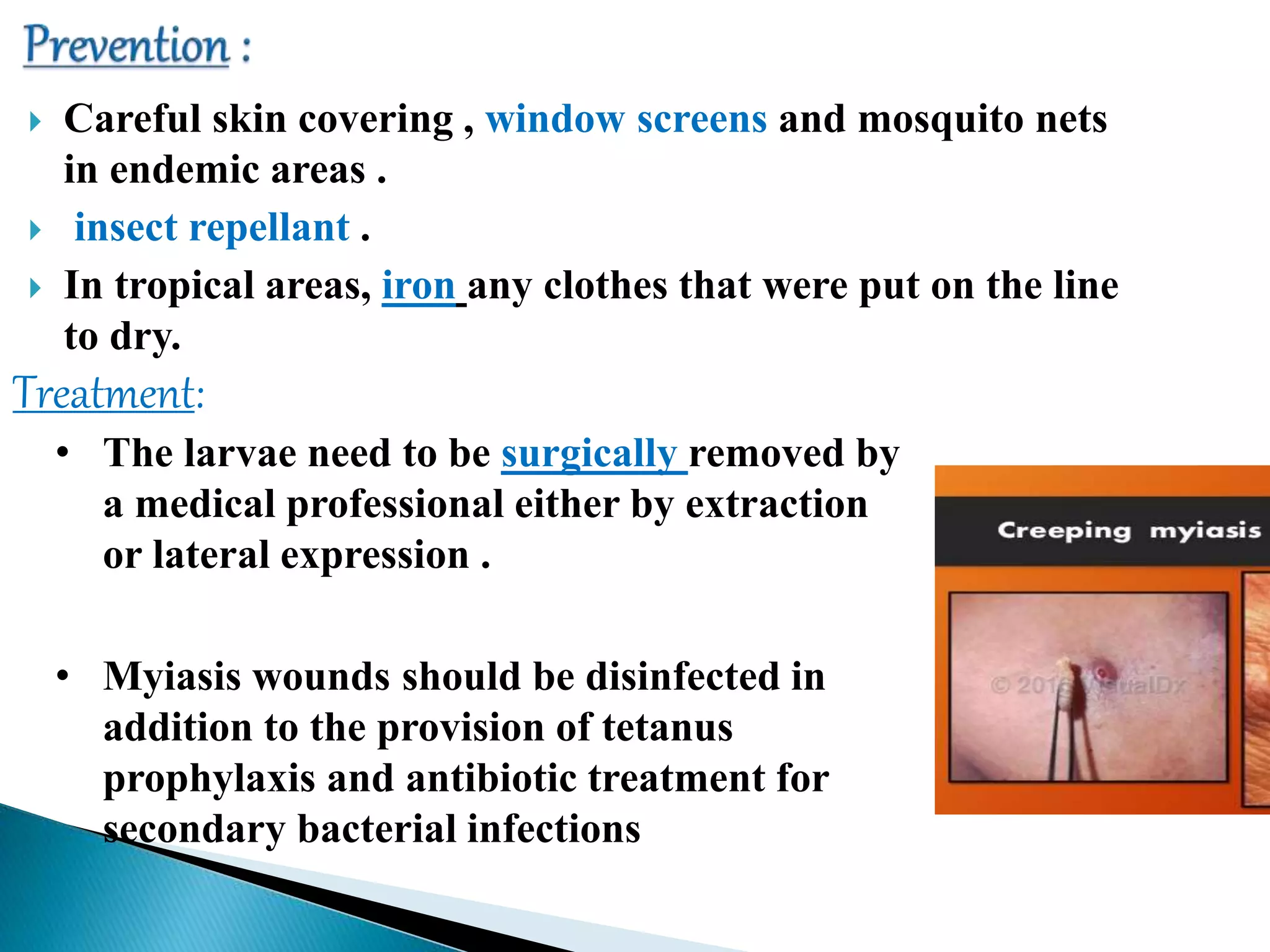
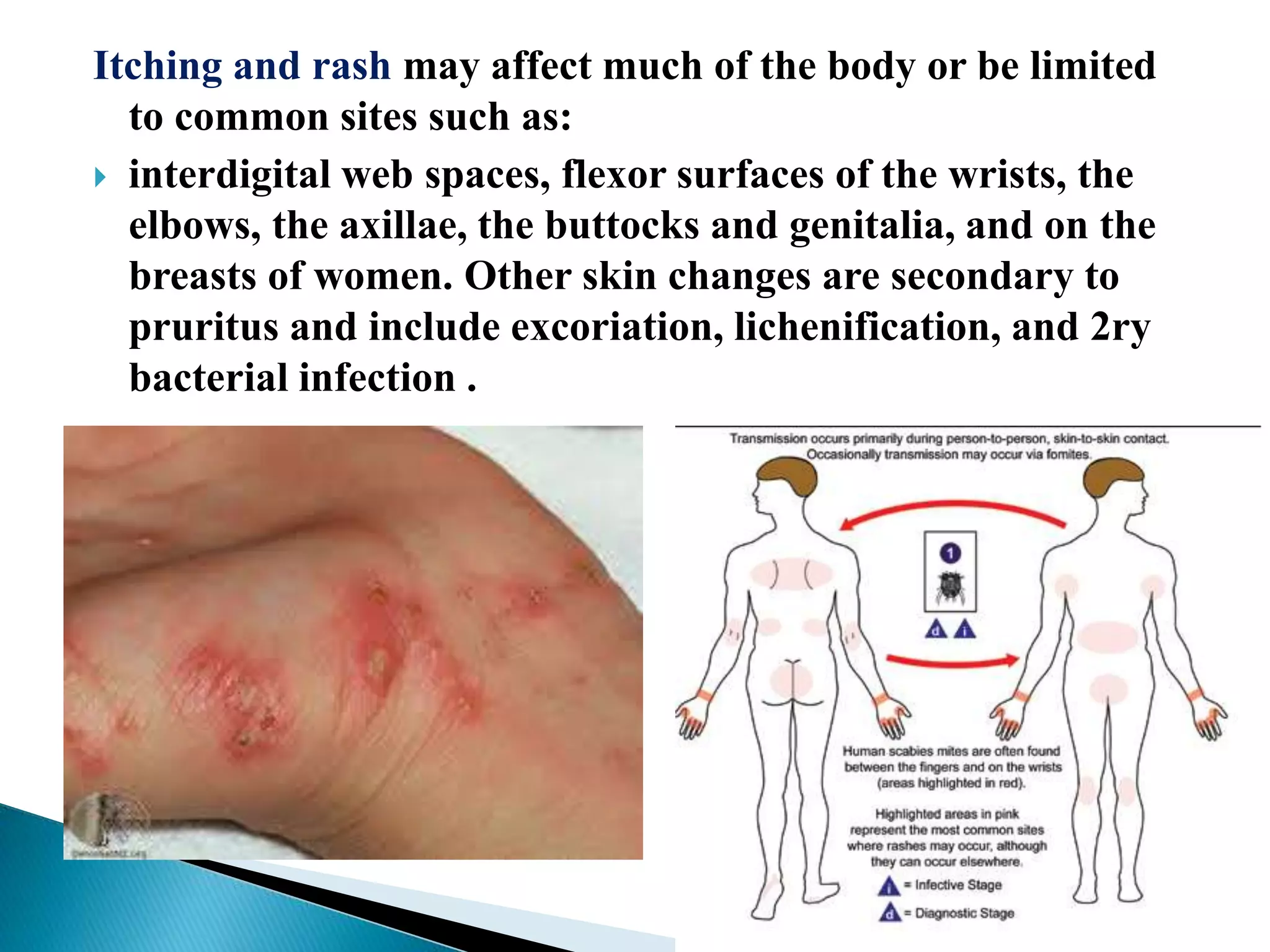
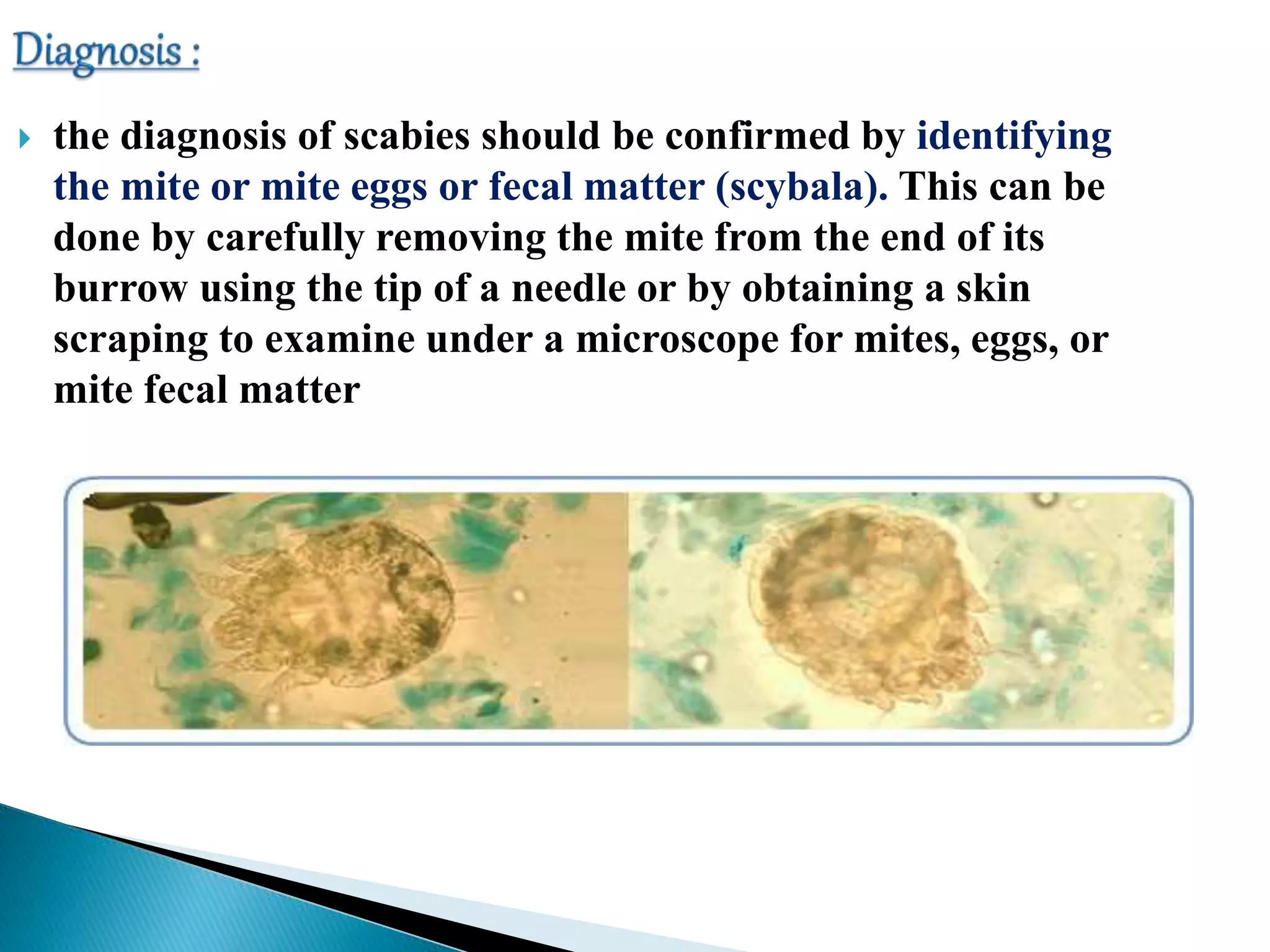
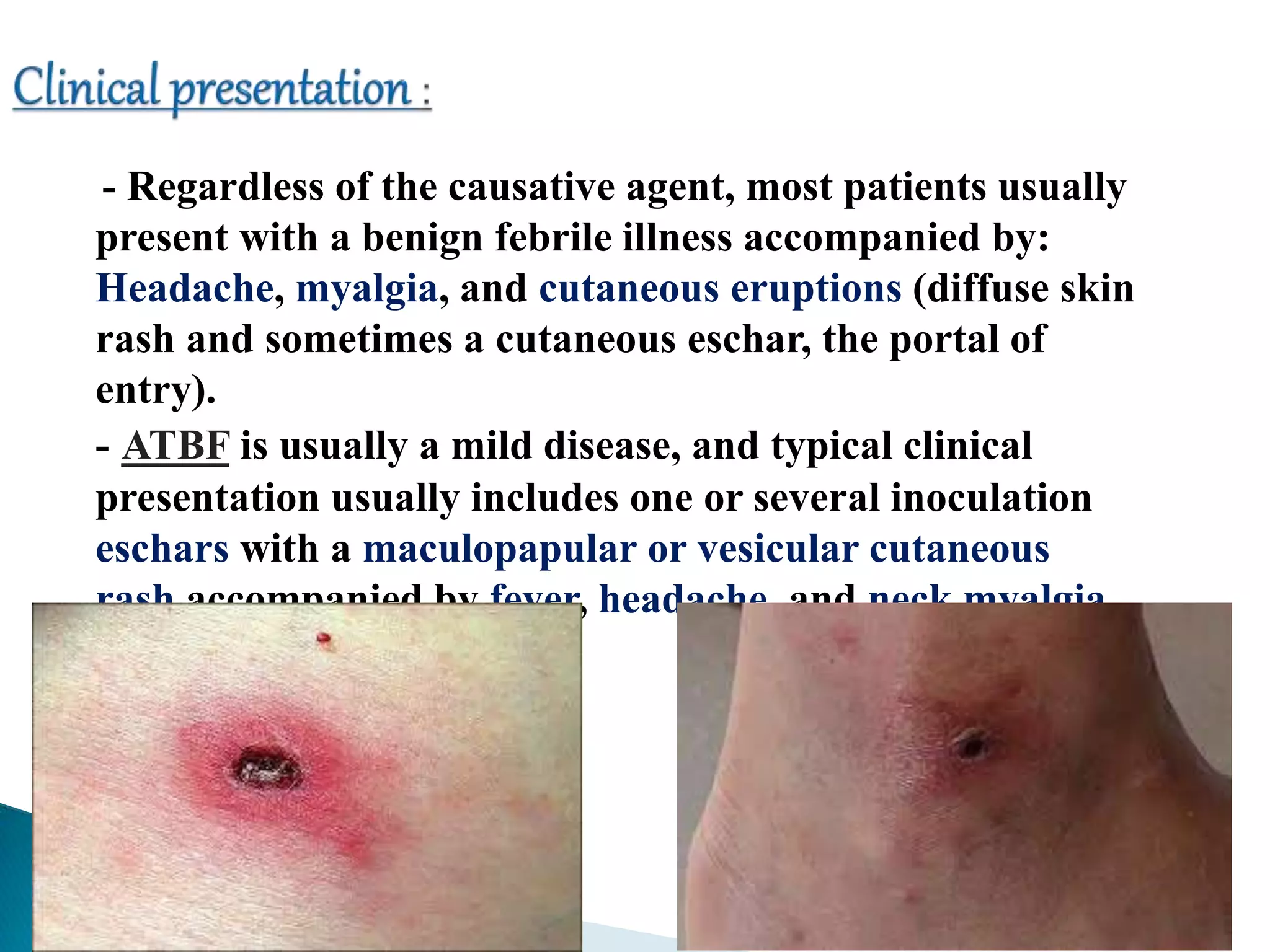
According to the document, common skin infections and lesions in travelers include insect bites and resulting bacterial infections, cutaneous larva migrans, leishmaniasis, myiasis, tungiasis, scabies, and arboviral infections. Dermatological disorders are frequently among the most common health problems in returning travelers. Diagnosis and treatment of these infections involves identifying the causative agent through methods like microscopy, culture, PCR, and responding with antibiotics, anthelmintics, or supportive care depending on the infection.