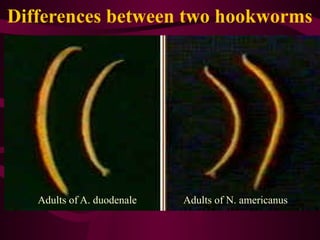
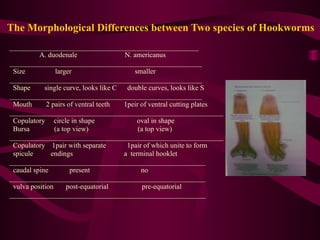
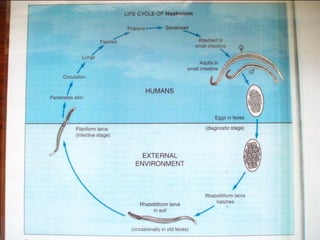
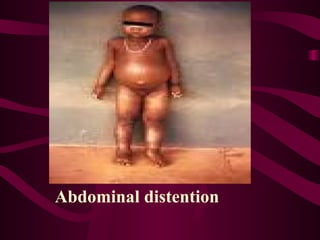
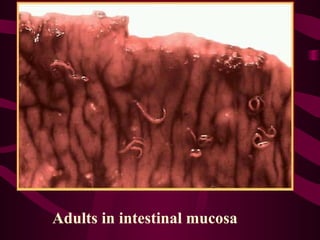
Hookworms, primarily Ancylostoma duodenale and Necator americanus, are intestinal parasites causing significant morbidity, particularly in tropical regions where they lead to anemia by feeding on host blood. The infection manifests through various symptoms, including cutaneous larva migrans, respiratory issues during larval migration, and gastrointestinal disturbances as adult worms reside in the intestines. Affected populations mainly include school-aged children, the malnourished, and pregnant women, necessitating effective diagnostic and treatment measures.