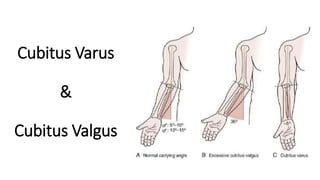
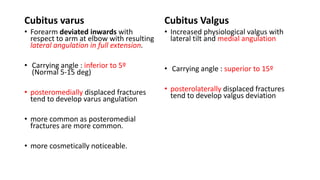
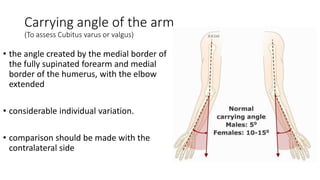
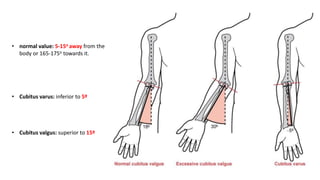
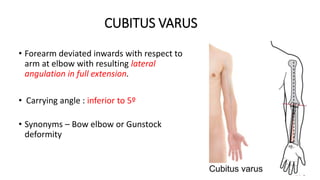
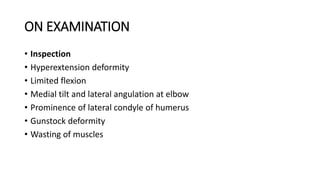
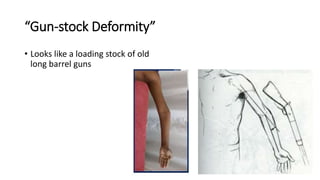
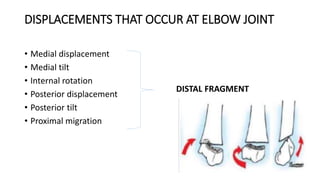
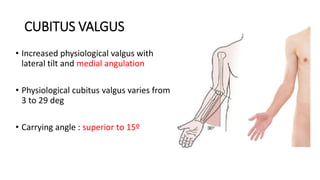
Cubitus varus and cubitus valgus are the most common complications of supracondylar humeral fractures in children. Cubitus varus causes the forearm to deviate inward with lateral angulation at the elbow joint. Cubitus valgus causes increased physiological valgus of the elbow. Both deformities can be treated with corrective osteotomy to realign the elbow if causing functional limitations or cosmetic concerns. Left untreated, cubitus valgus can sometimes lead to tardy ulnar nerve palsy due to nerve stretching over time.