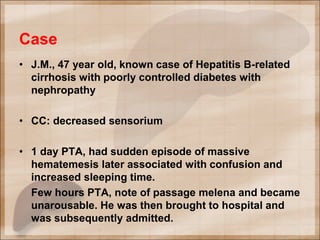
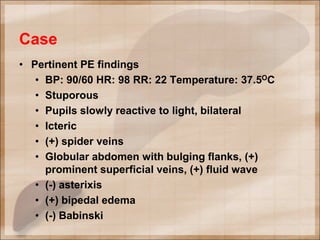
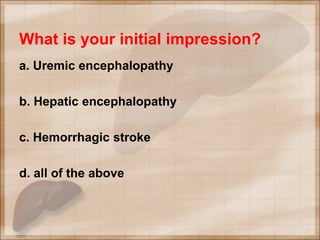
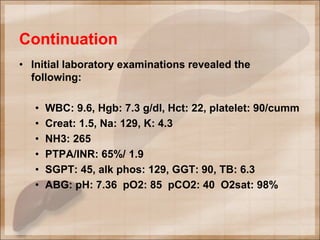
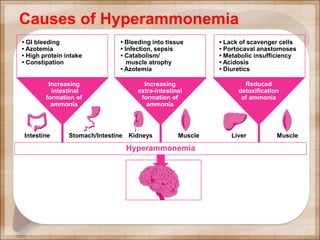
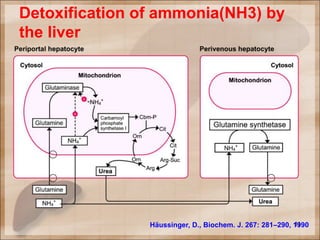
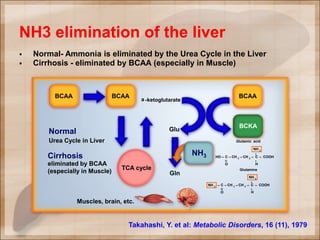
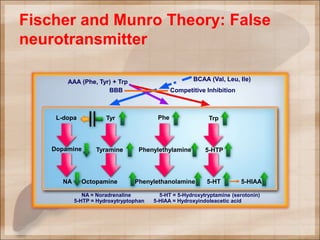
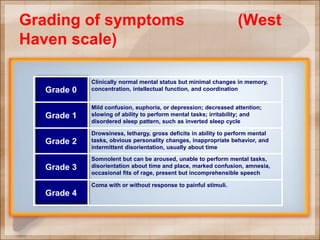
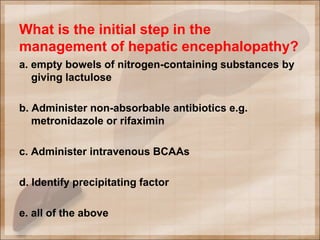
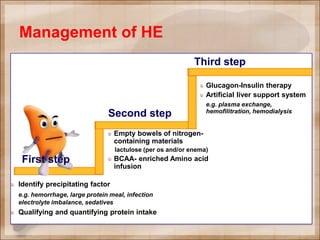
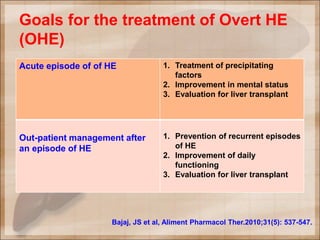
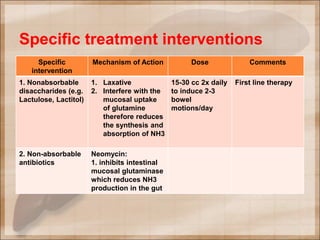
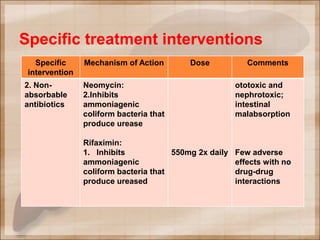
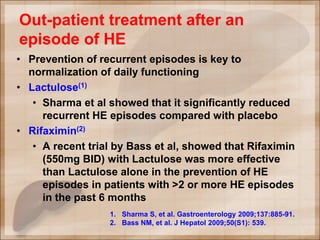
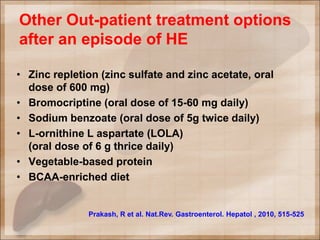
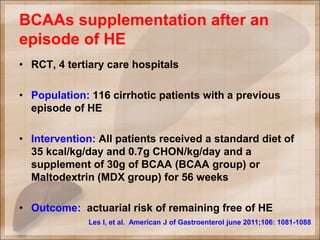
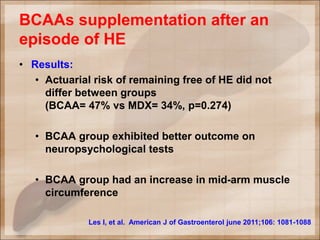
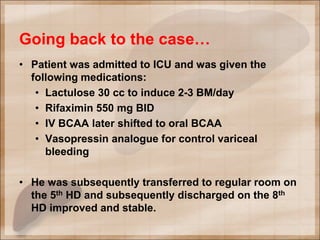
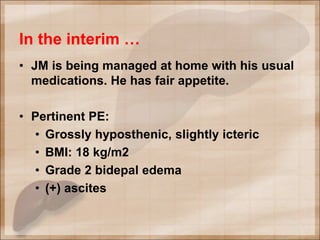
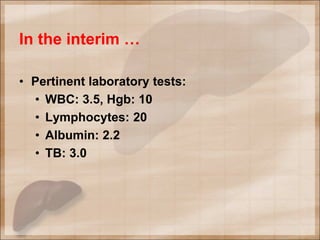
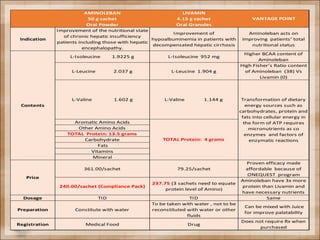
The patient, a 47-year-old man with hepatitis B-related cirrhosis and diabetes, presented with decreased sensorium after an episode of hematemesis. On examination, he was stuporous with signs of hepatic dysfunction. Laboratory tests found elevated ammonia levels. He was diagnosed with hepatic encephalopathy secondary to upper GI bleeding from esophageal varices. Treatment included lactulose, rifaximin, IV BCAAs, and a vasopressin analogue. He improved and was later discharged on oral BCAA supplementation for outpatient management to prevent recurrent episodes. On follow-up, he showed signs of protein-calorie malnutrition.