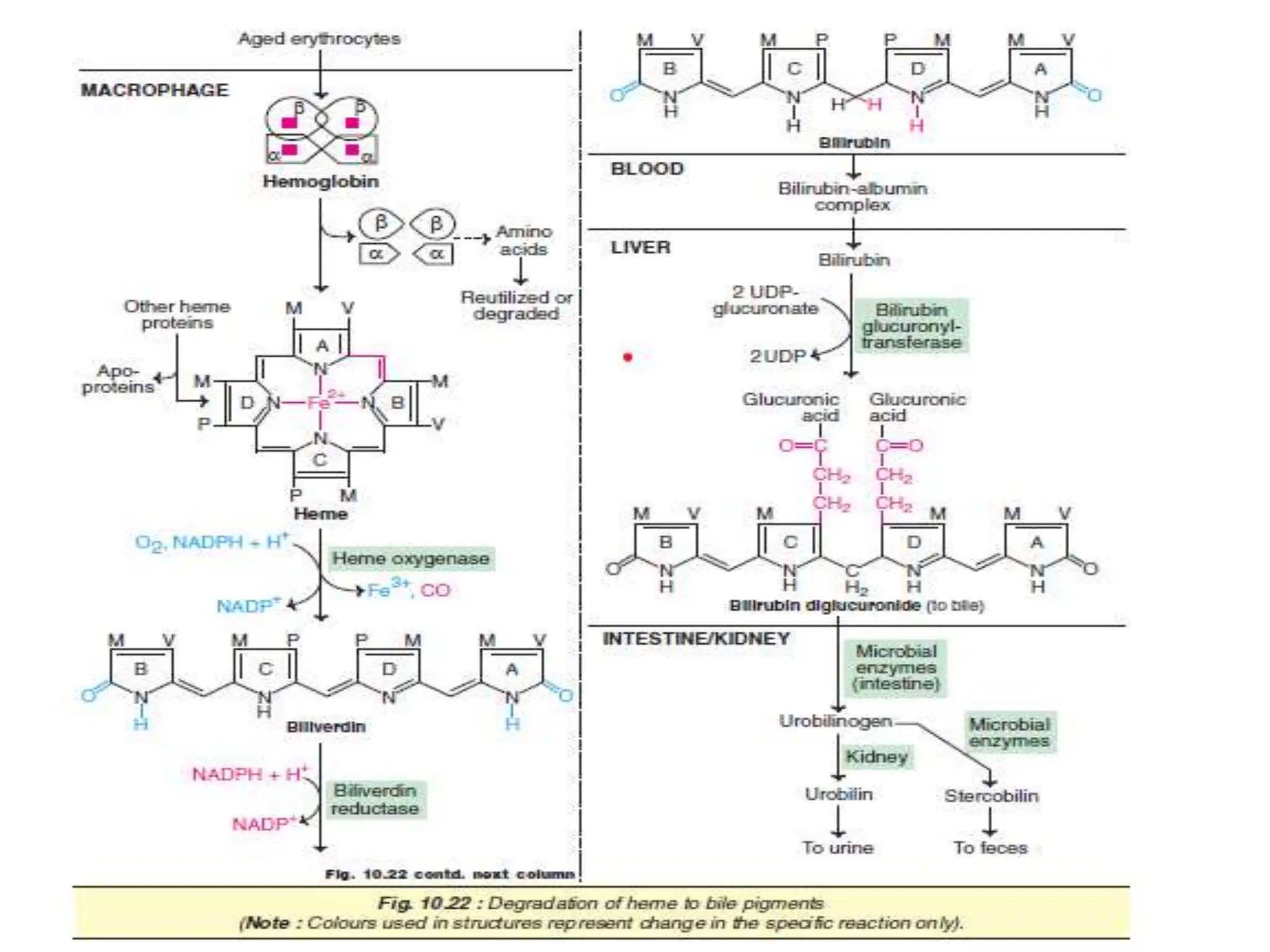
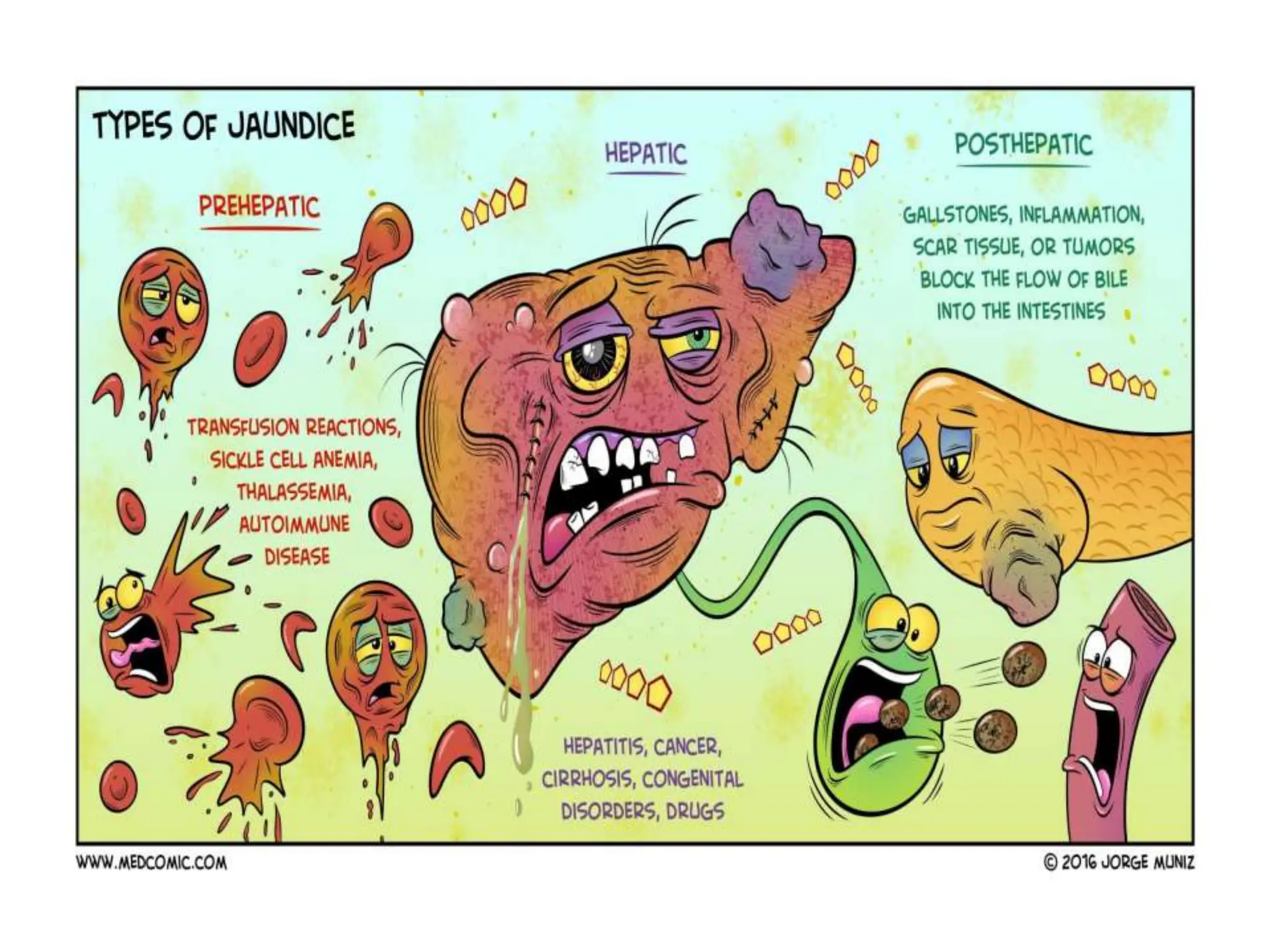
The document discusses heme degradation and the formation of bilirubin, detailing the processes involved from the breakdown of red blood cells to the excretion of bilirubin in bile. It explains the transport and conjugation of bilirubin in the liver, along with the fate of bilirubin in the body, and describes jaundice types including hemolytic, hepatic, and obstructive jaundice. Additionally, it covers genetic defects related to jaundice such as Crigler-Najjar syndrome and Gilbert's disease.