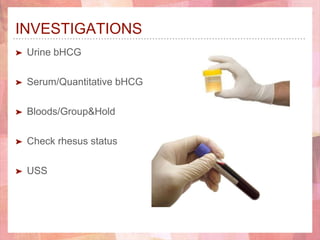
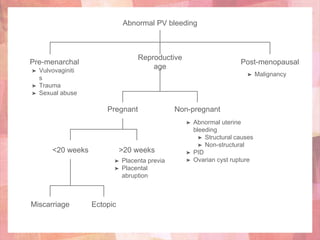
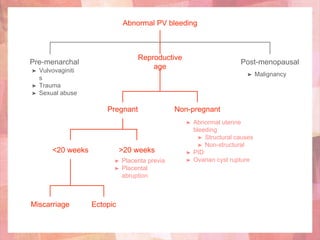
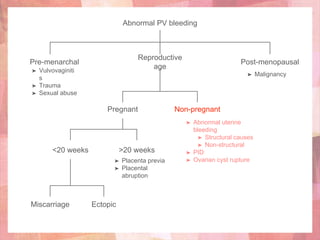
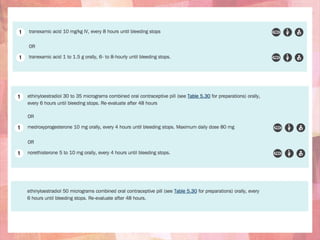
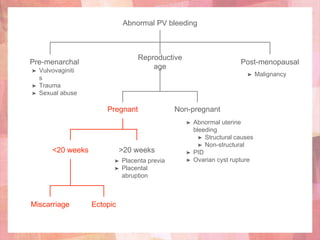
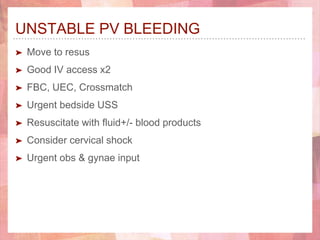
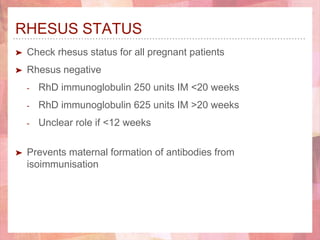
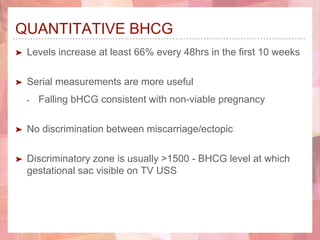
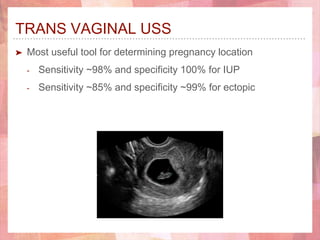
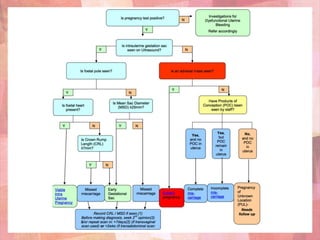
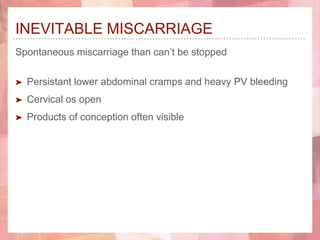
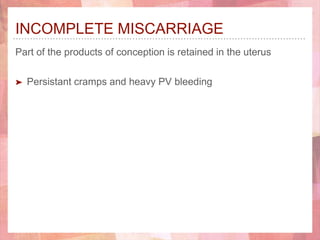
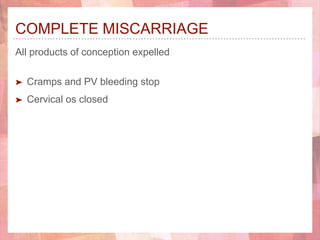
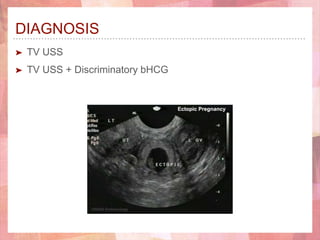
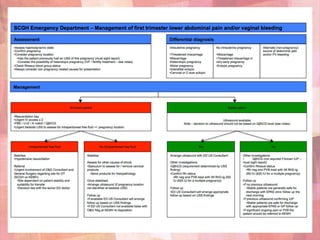
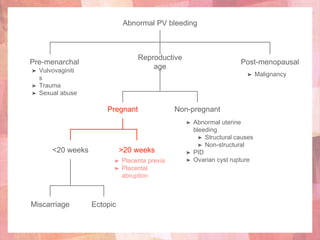
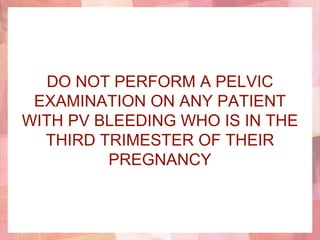
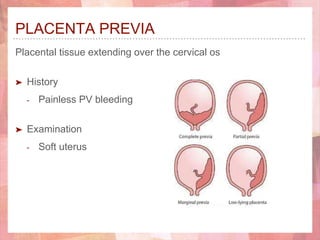
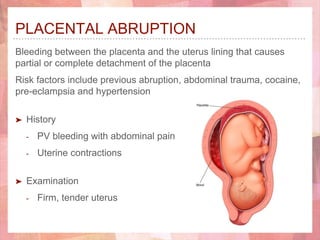
This document provides guidance on managing abnormal vaginal bleeding in the emergency department. It outlines how to assess patients presenting with vaginal bleeding, including determining if they are pregnant and stable. Common causes of vaginal bleeding are discussed for different age groups and pregnancy statuses, such as miscarriage, ectopic pregnancy, and issues later in pregnancy like placenta previa. Recommendations are provided on investigations, treatment options, and discharge criteria depending on the identified cause. Pelvic exams are not recommended for those in the third trimester due to risk.