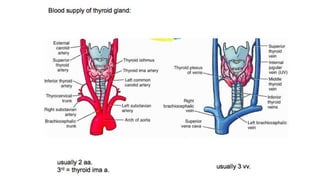
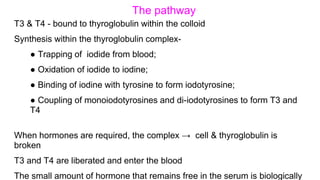
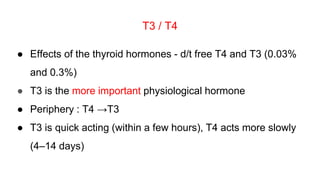
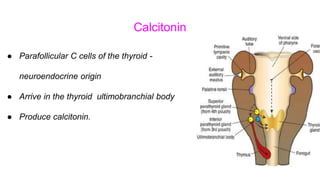
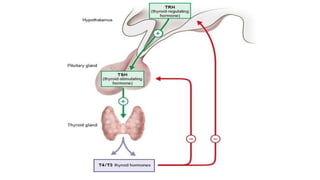
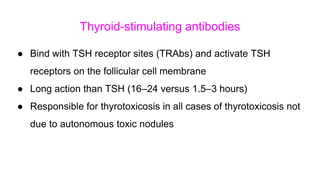
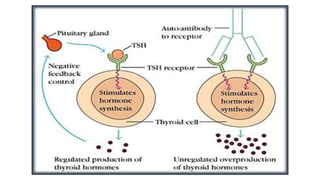
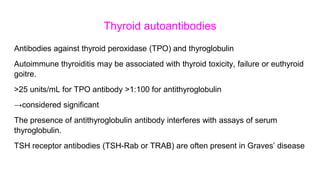
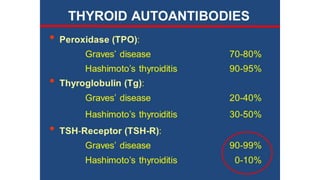
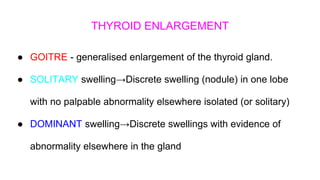
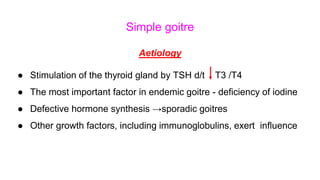
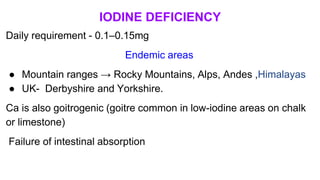
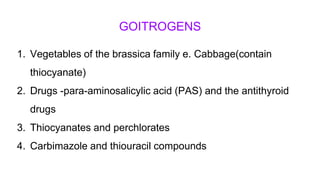
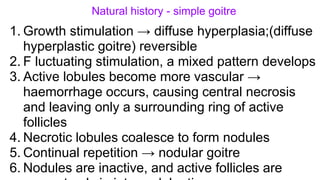
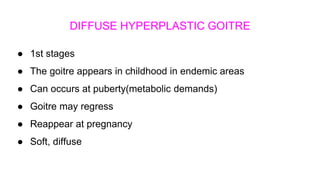
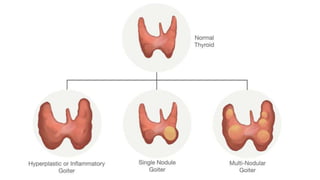
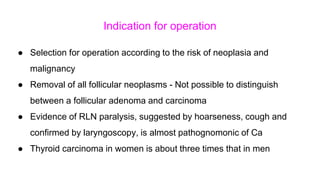
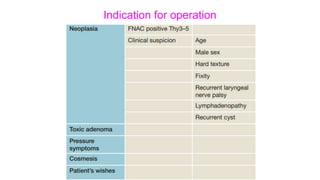
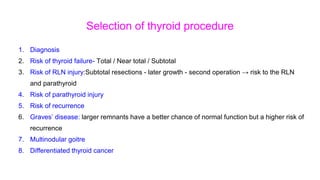
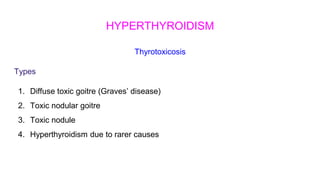
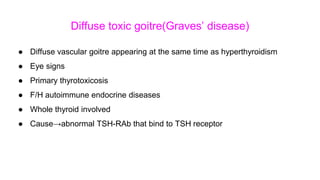
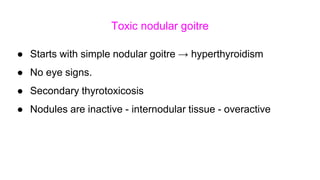
1. The document discusses the anatomy and physiology of the thyroid gland, pathophysiology of thyroid disorders including hyperthyroidism and hypothyroidism, investigations for thyroid disorders, and treatment approaches for conditions like simple goiter, multinodular goiter, Graves' disease, and toxic nodular goiter.
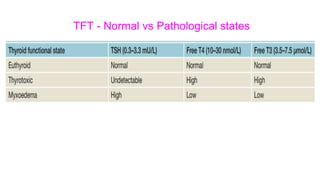
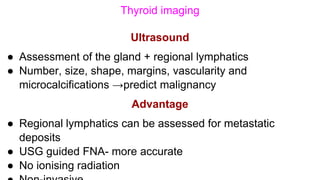
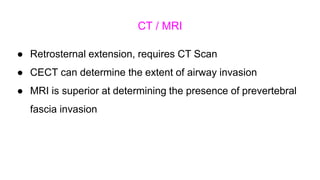
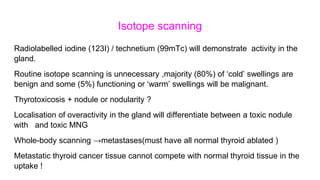
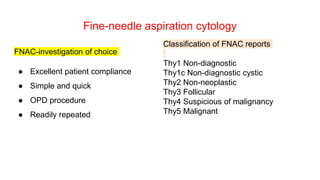
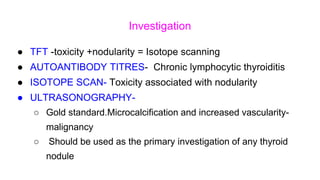
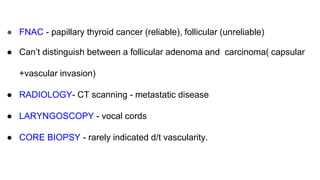
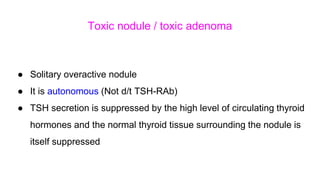
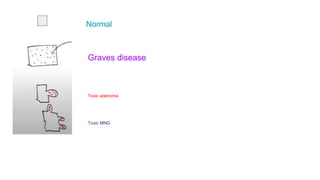
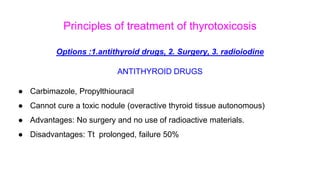
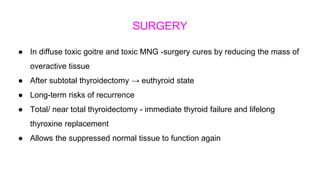
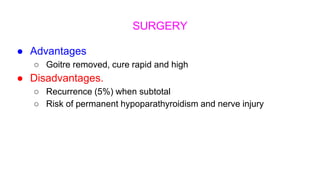
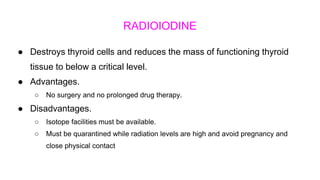
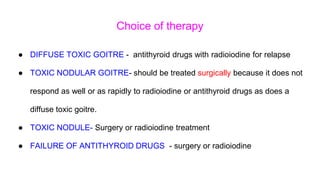
2. Key topics covered include the hormone synthesis and release pathways in the thyroid, investigations like ultrasound, isotope scanning and fine needle aspiration, and management options for hyperthyroidism like antithyroid medications, surgery, and radioiodine therapy.
3. Treatment approaches depend on the specific thyroid condition, with diffuse toxic goiter generally treated initially with antithyroid drugs or radioiodine,