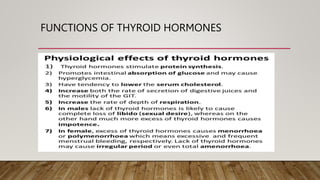
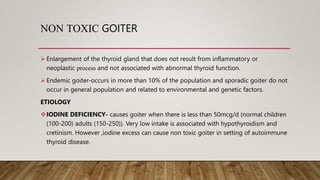
The document discusses the anatomy, embryology, histology, relations, blood supply, physiology, regulation of secretion, functions, and benign conditions of the thyroid gland. Some key points:
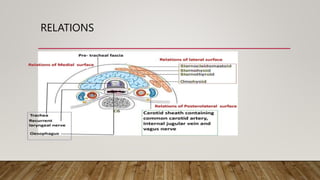
- The thyroid gland is a butterfly-shaped endocrine gland located in the neck, overlying the trachea. It weighs 20-25g and is larger in females.
- It develops from endodermal cells in the floor of the pharynx and forms as a diverticulum that elongates into the thyro-glossal duct.
- The gland contains follicles composed of epithelial cells and colloid containing thyroglobulin, the precursor of thyroid hormones.
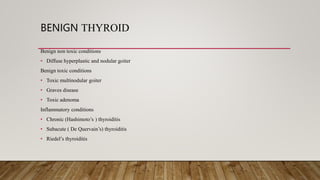
- Benign conditions include non




























































![CONT..
Regional and distant lymphadenopathy is common
FNAC is useful to diagnose the condition (Often trucut biopsy).
Chemotherapy is the mainstay of treatment. Doxorubicin or CHOP (i.e.
cyclophosphamide, hydroxydaunomycin, Oncovin [vincristine], prednisone) is the
commonly used chemotherapeutic regimen.
Rarely, total thyroidectomy is done to enhance the results.](https://image.slidesharecdn.com/thyroidgland1-231005071359-bdb08841/85/THYROID_GLAND-1-pptx-88-320.jpg)