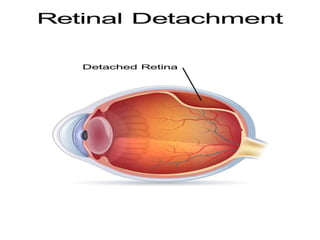
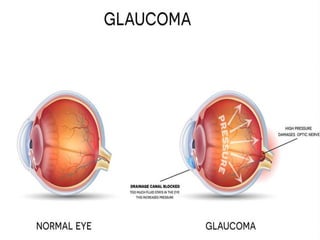
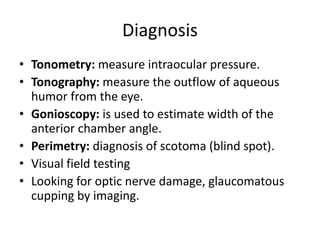
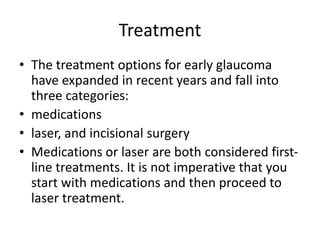
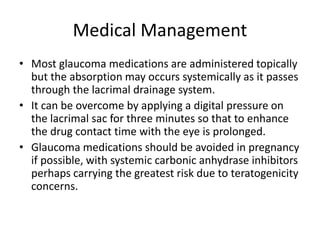
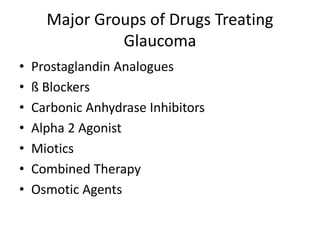
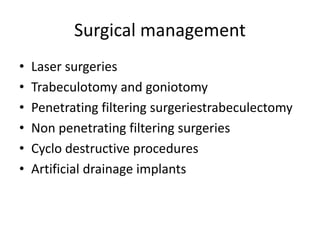
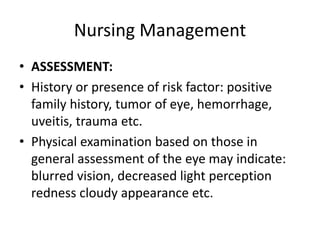
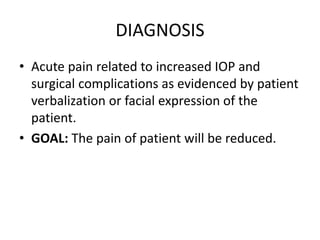
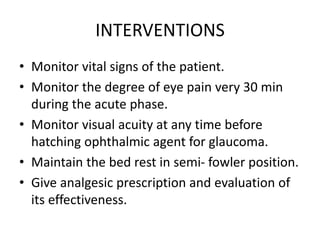
The document discusses retinal detachment and glaucoma, detailing their types, causes, symptoms, diagnosis, and treatment options. Retinal detachment occurs when the retina separates from its supporting tissue, with common causes including age and diabetes, while glaucoma is characterized by optic nerve damage typically linked to increased intraocular pressure. Management strategies include medical, surgical, and nursing interventions aimed at preventing vision loss and addressing complications.