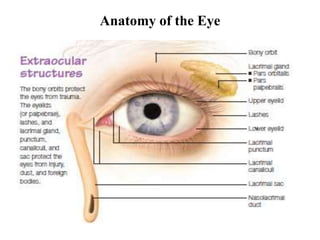
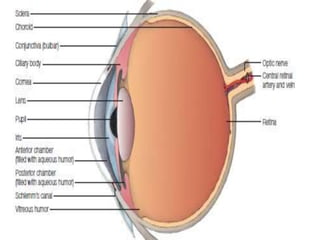
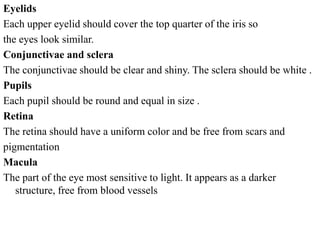
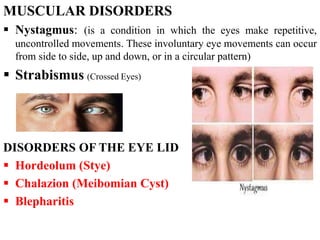
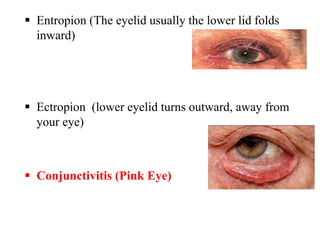
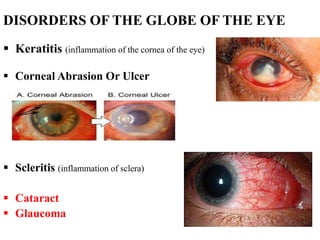
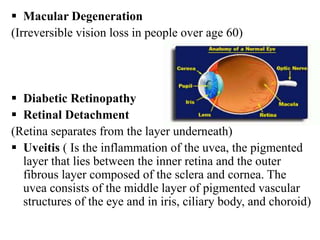
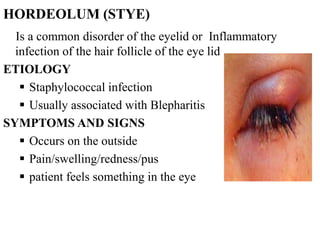
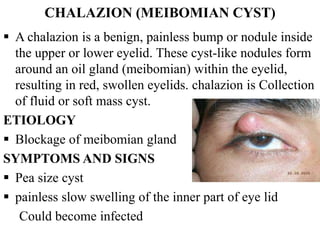
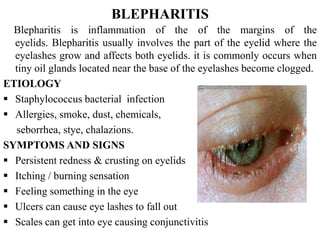
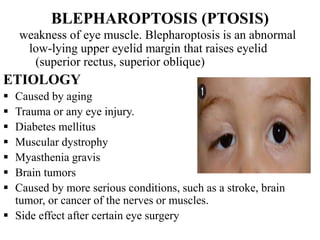
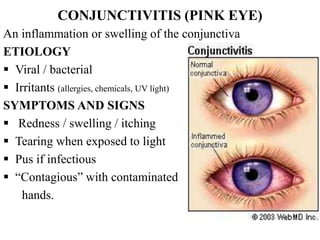
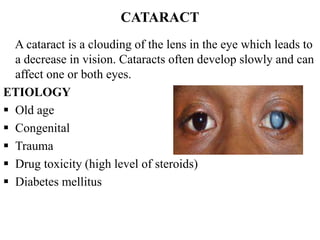
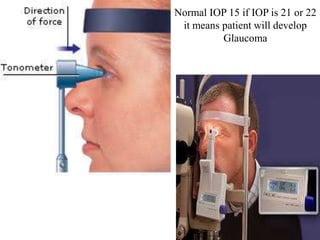
The document outlines various eye disorders, including refractive errors, muscular disorders, eyelid disorders, and globe disorders, detailing their characteristics, symptoms, and treatments. Specific conditions such as hordeolum, chalazion, blepharitis, conjunctivitis, cataracts, and glaucoma are addressed, with emphasis on their etiology, diagnosis, and management options. The text serves as a comprehensive guide for understanding the anatomy of the eye and the associated disorders affecting vision.