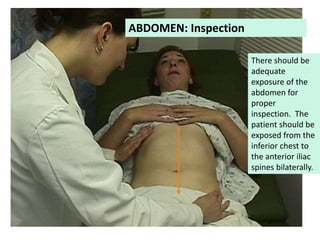
This document provides guidance on performing a clinical examination of the abdomen, including inspection, auscultation, percussion, and palpation techniques. It describes how to evaluate the abdomen by listening for bowel sounds and vascular bruits, percussing to determine organ sizes and detect dullness or fluid, and palpating the liver, spleen, kidneys, and aorta. The document emphasizes performing auscultation before percussion or palpation, and outlines specific examination techniques and signs to evaluate for common abdominal conditions.